Introduction
Some health problems that cause suffering and require expensive health care services are the result of age-related risk factors that are amenable to prevention-oriented interventions. Examples include fall-related injuries, pressure ulcers in immobile patients, and malnutrition. But all too often, professionals and organizations that provide care to seniors do not address these risk factors before injury or other adverse conditions occur. In Sweden, the Senior Alert program, a national preventive care dashboard for the elderly, was developed to address these issues.1 Senior Alert began a decade ago in one county in Sweden and has now spread to all 21 counties and almost all municipalities.2
In the early 2000s, Göran Henriks and colleagues at Qulturum3 in Jönköping County were inspired by the Robert Wood Johnson Foundation’s Pursuing Perfection program4 to improve care through system redesign and process improvement. Qulturum developed Senior Alert, a quality improvement registry aimed at reducing health risks faced by older people. As implemented in Sweden, Senior Alert screens individuals for certain risks, determines actions that could reduce identified risks, and follows up with patients and providers regarding implementation of risk-reduction plans. Thus, Senior Alert is both a) a quality improvement registry in which the health status of registered patients is followed over time, and b) a preventive care process.
Before the launch of Senior Alert, Sweden already had research-oriented disease and procedure registries, but Senior Alert was the first registry aimed at reducing health problems and improving accountability. Senior Alert also acknowledges the important role of nurses, who traditionally had no decision-making role in care improvement efforts, even though their work was central to prevention of common health problems in the elderly population.
Senior Alert initially focused on falls, pressure ulcers, and malnutrition — three conditions for which screening tools and risk-reduction potential were supported by the research literature. An option to include oral health was added later; the program can be adapted to include other conditions.5
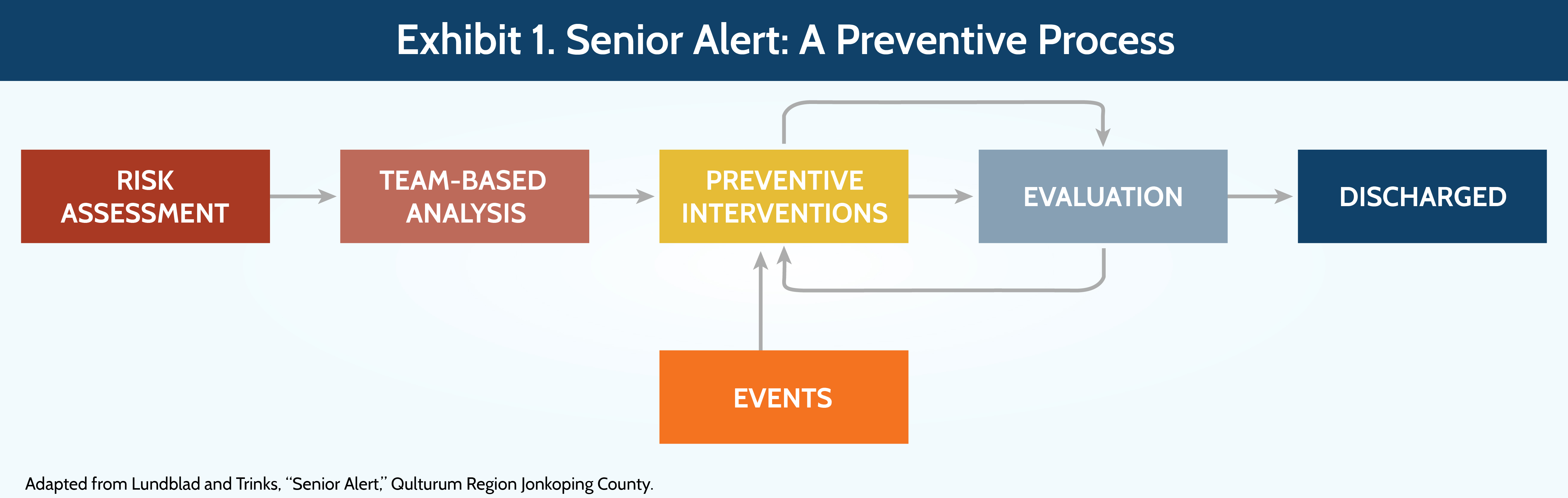
The prevention process begins with risk assessments. For patients found to be at risk, a prevention plan is developed, implemented, and evaluated (Exhibit 1). These steps happen quickly. Typically, the risk assessment and implementation of the prevention plan all occur on the same day. Information about all steps is entered into a national Senior Alert database — the largest quality registry in Sweden.
Key Program Features
Risk Assessments
Risk assessments are built into various care routines in hospitals, primary care practices, and home and nursing home care settings in which patients receive care. The screening tools, which have all been validated in published research,6 are composed of six to 10 scalable questions. One of Senior Alert’s innovations was to put the screening tools for falls, pressure ulcers, malnutrition, and oral health into a single instrument, which eases administration and makes use of overlapping content. No blood tests or special examinations are required. The risk assessment takes about 10 to 15 minutes to administer and may be done by nurses, nursing assistants, physical therapists, or other personnel.7 Risk is determined based on patients’ scores on each scale.
Criteria for repeat screening vary by type of service unit and nature of risk. For example, patients are screened at every hospital admission. Nursing home patients are screened at least every six months, although certain circumstances (e.g., sleeping problems) may trigger an earlier screen. Home care patients are rescreened at least once a year.
Development and Implementation of Care Prevention Plans
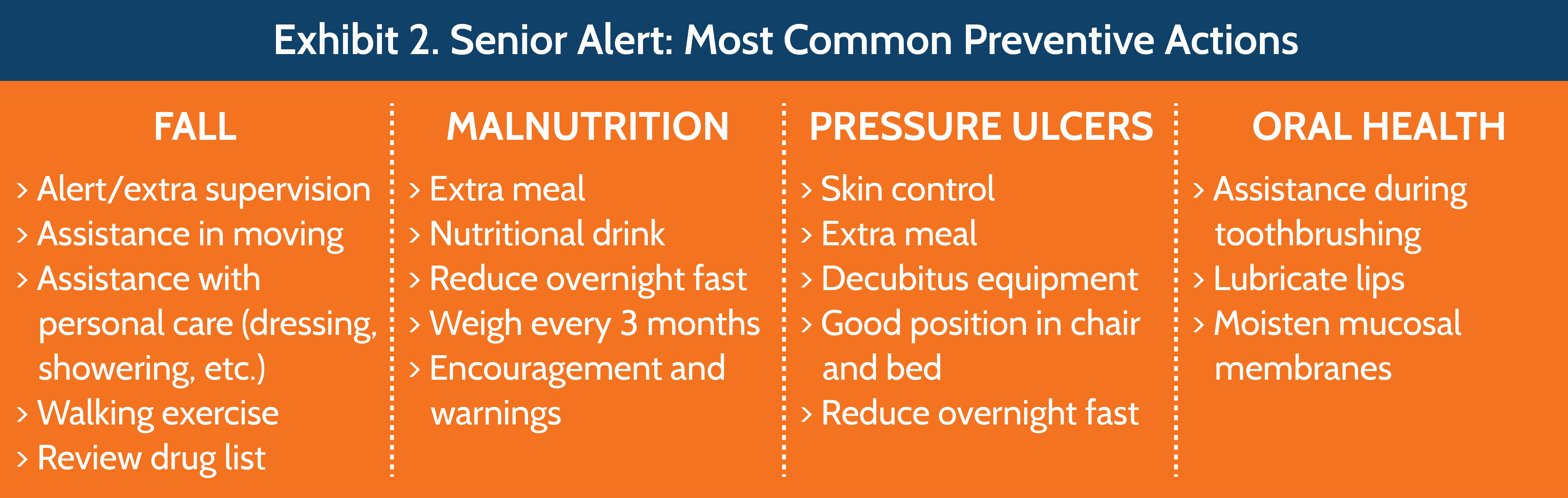
Teams based in care units analyze the results of the risk assessments. The teams are typically led by nurses and may include nurse assistants, physiotherapists, occupational therapists, dieticians, and physicians. If a patient is at risk, the team develops a specific preventive action plan, drawing from a menu of 100 possible interventions — about 25 for each risk (Exhibit 2). Once the interventions are identified, the team decides which professionals (e.g., nurse, physical therapist) should be involved.
Information about a patient’s risks and action plan is entered into the Senior Alert registry. All personnel in the organization have access to this information. Risk assessments and action plans are revisited periodically in settings where patients have long stays.
Follow-up varies by settings. The whole process happens rapidly in the hospital, where a risk assessment is done soon after admission and an action plan is quickly developed and implemented. Information about weight is entered at discharge, along with whether the patient had a fall or developed a pressure ulcer. In nonhospital settings, the team can compare an earlier screen with a new one for risks like oral health and weight loss.8 Information about falls, pressure ulcers (location and severity), and weight loss are to be recorded if they occur. Regarding falls, information about the time of day (five categories) and consequences (10 types of injuries) are entered in the register for use in identifying patterns that could be addressed by providers or policymakers.9 (Privacy law prevents linking the patient’s electronic health record with the registry, which could supplement data capture about incidents.)
The data can be used for three distinct purposes. One is in the care of individual patients — for example, to create a prevention plan for a patient at risk. Providers can see whether a patient has one of the specified risks, whether a prevention plan exists, and whether there has been follow-up or incidents have occurred. Second is for quality improvement purposes in care organizations. Providers or policymakers can see the number and types of risks for which a prevention plan is not in place at the organizational or county level and take remedial action. Third, a dashboard in the Senior Alert management portal can show comparisons across geographic areas and over time, providing an impetus for improvement or further research. Local, regional, or national trends also can be shown. None of this information existed before Senior Alert.
Organization
Senior Alert operates with a staff of five or six people at Qulturum and two to three people at the Uppsala research center, which maintains the register and analyzes results. Qulturum staff, supplemented by additional coaches, coordinators, and webinars, have educated some 5,000 individuals and 900 care improvement teams at service units throughout the country. The training includes: screening patients; entering data into the register; planning and implementing prevention plans using quality improvement methods; and using the registry to analyze results. Personnel in many service units — particularly nursing homes and home care — had never used or interpreted data before, and many had never before worked in teams.10

Participation by counties, municipalities, and service units was facilitated by incentive funding from a national campaign called “Better Life for Sick Elderly” that began in 2010. Those incentives ended in 2014, but counties and municipalities are continuing with Senior Alert, which is free to users. It has a budget of about $470,000.11 This does not include the costs incurred by participating service units, though leaders at Senior Alert believe that when the program is implemented properly, there will be net savings in personnel time resulting from the prevention of adverse events.12
Results
- Almost 1.4 million risk assessments (from about 520,000 patients)13 went into the database from 2009 to late 2015.14 About 40,000 risk assessments are added to the database monthly.15
- Eighty-three percent of risk assessments conducted in 2014 showed a risk, ranging from 23 percent risk of a pressure ulcer to 66 percent risk of falls. Many patients had more than one risk.16
- Overall, data show that preventive action plans were developed for approximately 80 percent of patients with an identified risk.17 Data at the county council level — mostly hospital patients — show that 90 percent of patients at risk received at least one preventive action and evaluation in 2014, up from 83 percent in 2009.18 At the municipality level — nursing homes and home care settings — the rate increased from 53 percent to 77 percent.
- Between 2011 and 2014, data from Senior Alert19 show: a 30 percent reduction in falls,20 a decline in the incidence of pressure ulcers from 14.3 percent of patients to 9.4 percent, and a decline in the incidence of weight losses greater than 5 percent of total body weight from 14.3 percent of patients to 12.5 percent.21
Senior Alert has enhanced health system performance by improving the way the system responds to the needs of patients. Health professionals have access to information and intervention strategies that did not exist in any standardized and systematic way before the program was implemented. The spread of expertise in quality improvement and preventive care across health care organizations throughout the country is another benefit of the program.
The leadership of Senior Alert describes a culture change in the participating organizations over the past five years, where staff have realized that data can be collected and used in a team approach to prevent many adverse events among elderly patients.22
Challenges
Leadership and commitment are needed at each organization, and not all organizations may appreciate the overall benefits.23 Senior Alert involves a complex set of activities conducted in individual care units. Collection of outcome information is challenging. Compliance at the level of data entry is high, but there may not always be complete consistency between what goes into the registry and the reality on the ground. To address this, Senior Alert leads an audit once a year in every municipality, in all nursing homes and home care settings.
Sweden’s privacy law also creates challenges. Registries are separate from patients’ medical records, so the registry information is not automatically entered into medical records. Ideally, the preventive action plans would cross organizational boundaries.
An ongoing challenge for Senior Alert is whether it can remain an integral part of the health care system in the absence of funding from the government. If county councils believe that Senior Alert reduces the use of emergency departments or hospitals, then they may agree to provide funding tied to providers’ participation in the program. Early signs are positive. Only two municipalities have stopped participating since the national government funding ended.24 In addition, some new participants have joined, particularly private providers. Moreover, some municipalities are now requesting that Senior Alert develop an approach for mental health issues and for health care–acquired infections.

Potential for Replication in the United States
The screening and care prevention aspects of Senior Alert are readily adoptable by U.S. hospitals, nursing homes, and home care agencies and can be encouraged through economic incentives — such as Medicare’s imposition of penalties on health care organizations for the occurrence of “reasonably preventable” health care–acquired conditions. Although hospitals and other sites in the United States have screening and prevention tools in place, active leadership would be required for successful adoption of a program similar to Senior Alert.
The U.S. would do well to develop reporting arrangements that enable appropriate community actions to meet the needs of seniors, as Senior Alert does so well.
Geography poses a much greater challenge. In Sweden, Senior Alert allows for comparisons to be made across organizations and regions, as well as over time, but the registry must be maintained regularly and the data require a certain level of standardization. This may be difficult in a much larger country like the U.S., which also has a more complex health care system. It could be feasible, however, to implement a Senior Alert–type registry at the state level, in large health plans, or in organizations that operate multiple hospitals or nursing homes.
Joanne Lynn, M.D., the director of the Altarum Institute’s Center for Elder Care and Advanced Illness, in Washington, D.C., says that the United States has nothing as useful as the Senior Alert system to guide or monitor improvements in services for elderly people. The U.S. focuses on measuring quality elements like cancer screening, instead of focusing on the community at large. “The U.S. would do well to develop reporting arrangements that enable appropriate community actions to meet the needs of seniors, as Senior Alert does so well,” Lynn says.
However, it is not likely the U.S. will build a community approach to monitoring and managing senior care. “We have enabled dozens of cottage industries to serve disabled seniors, without requiring even interoperable reporting on needs and outcomes. Our supportive services are funded, led, and studied in pathways quite separate from medical services, and the former are starved while the latter are bloated,” Lynn says. Creating something like Senior Alert would require a willingness to innovate. In many U.S. cities today, the waiting list for home-delivered food is more than six months — longer than the lifespan of many on the list.
Conclusion
Senior Alert has shown that preventable risks are very common in the over-65 population. In addition, the program has shown that those risks are connected with each other and that a systematic approach can address the prevention of age-associated risks. The Senior Alert database of patient-specific information about risks, prevention plans, and follow-up information is a resource that can influence the care provided to patients; remind providers about prevention-related gaps in services; provide information about risks in the elderly population to management at different levels, including service unit, county, region, and nationwide; and provide information at each of those levels about the extent to which those risks are being addressed. Senior Alert also has demonstrated that important aspects of nursing care can be measured and made the subject of quality improvement, and it has contributed to a national discussion in Sweden about patients with high care needs.25 Although impact information is largely limited to before-and-after observational data, the available evidence suggests that much harm that can befall the elderly is being prevented.
For more information on health care for the elderly in Sweden, see the case study Sweden's Esther Model: Improving Care for Elderly Patients with Complex Needs.


