Overview
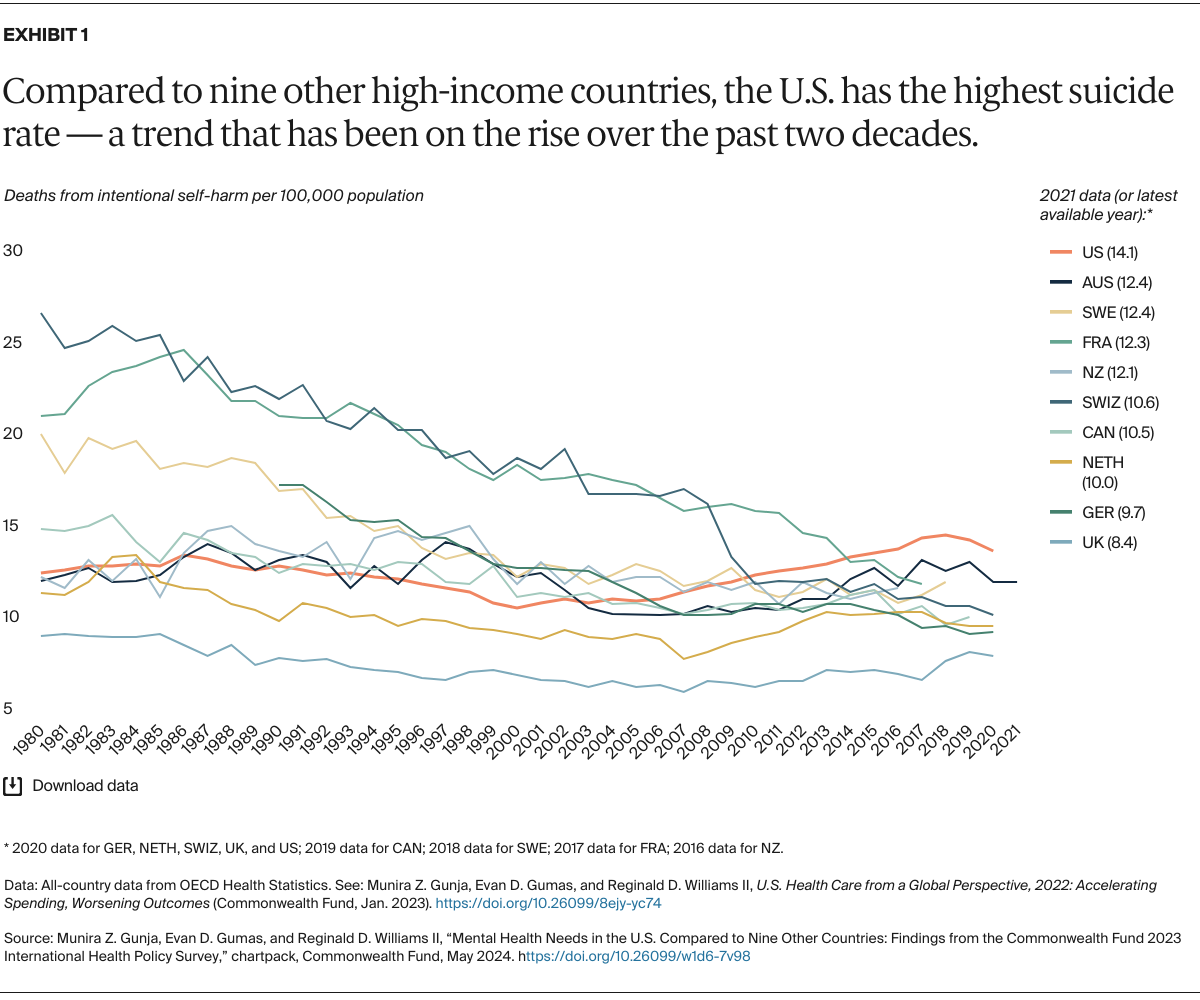
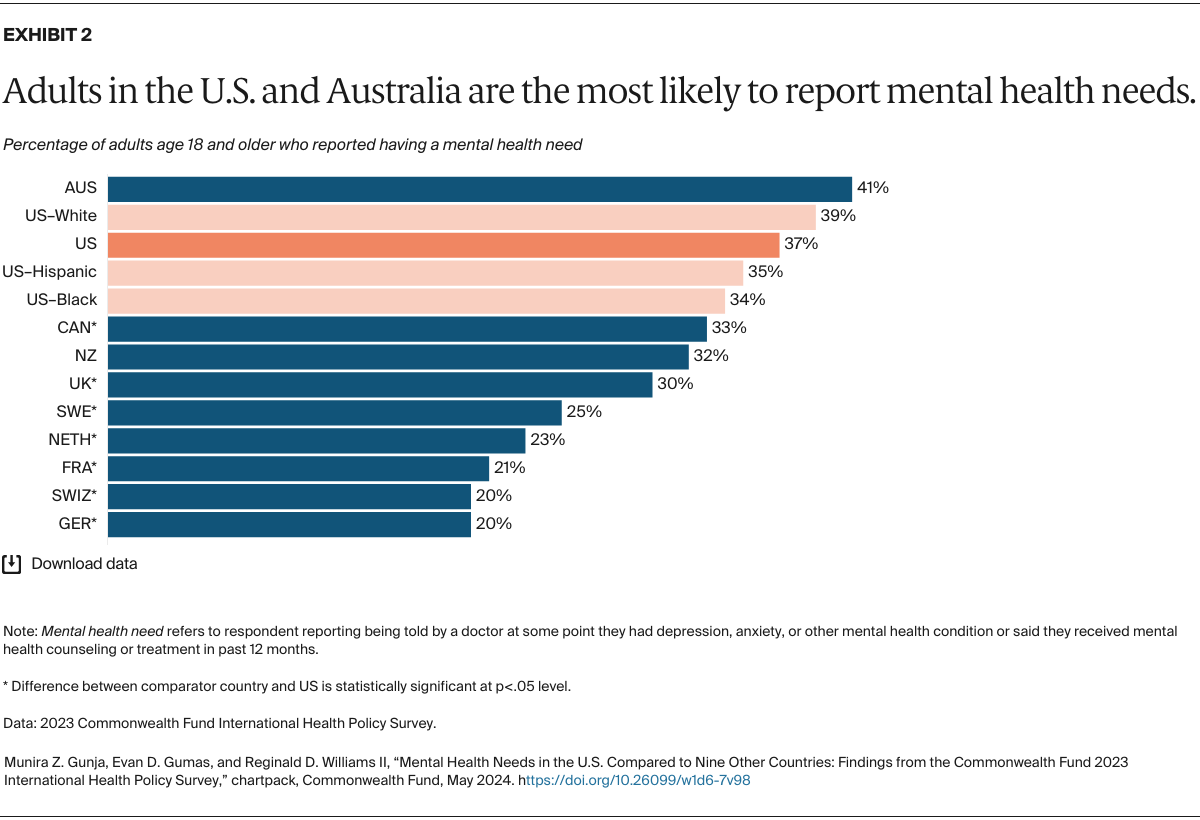
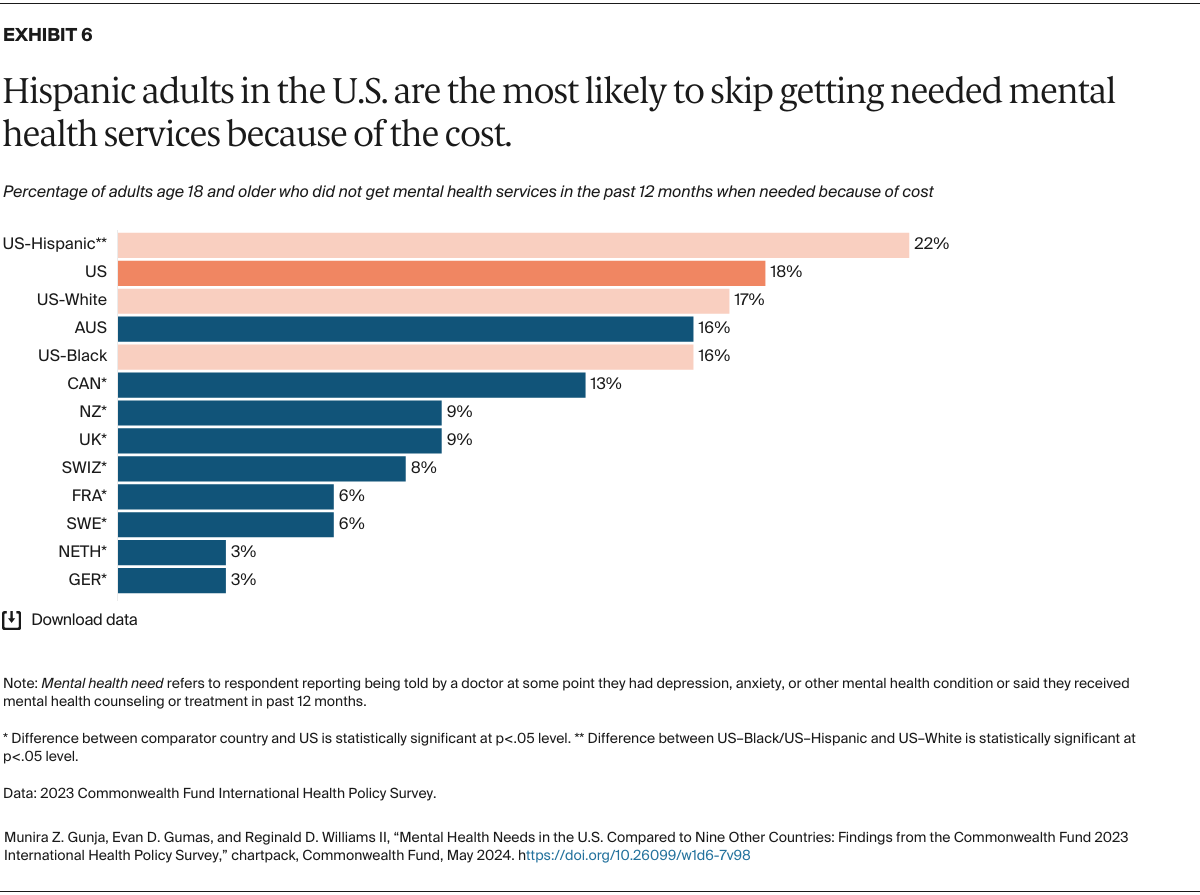
Like other high-income countries, the United States has experienced a rise in mental health conditions over the past four years. But unlike its peers, the U.S. does not guarantee access to affordable and comprehensive health care, including mental health care. Nearly a third of the 50 million U.S. adults with a mental health condition are unable to get needed treatment, and about 11 percent lack health insurance.
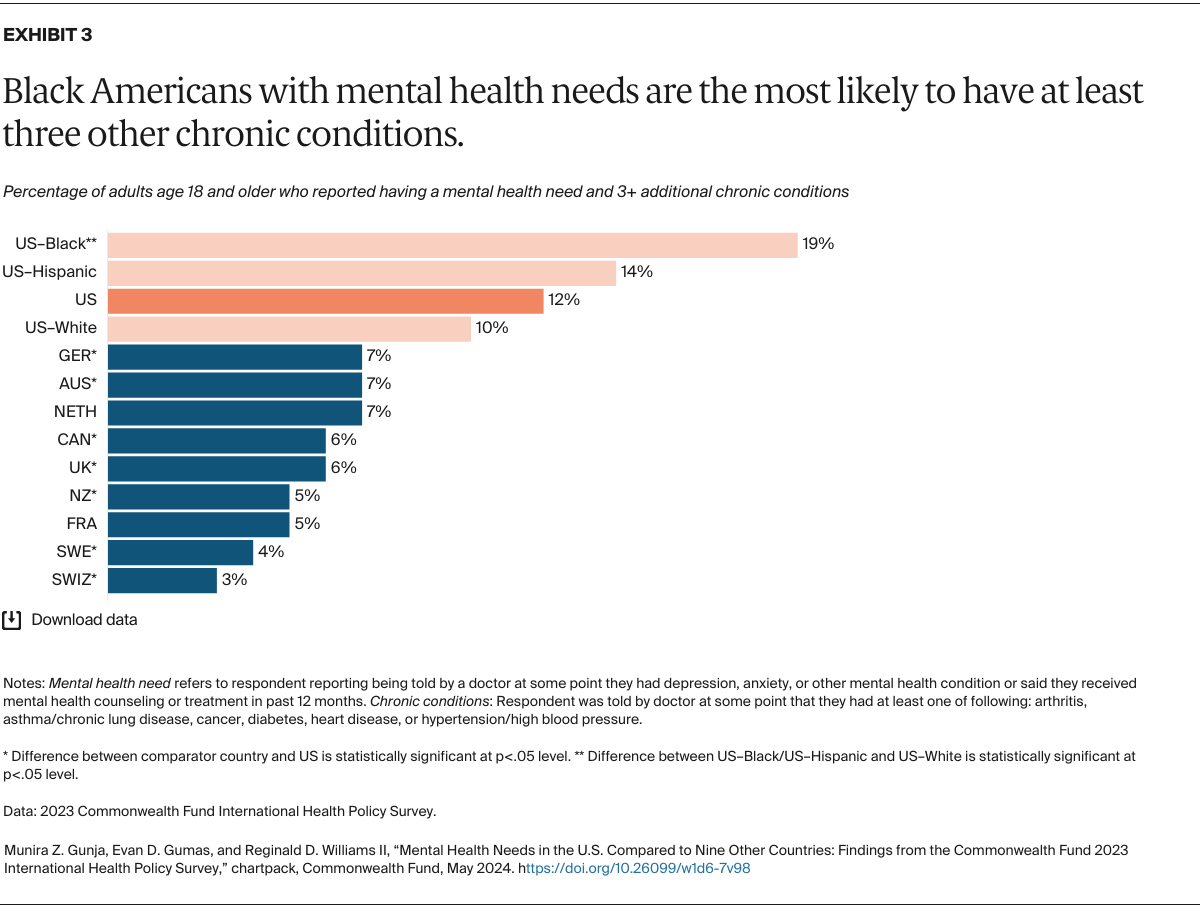
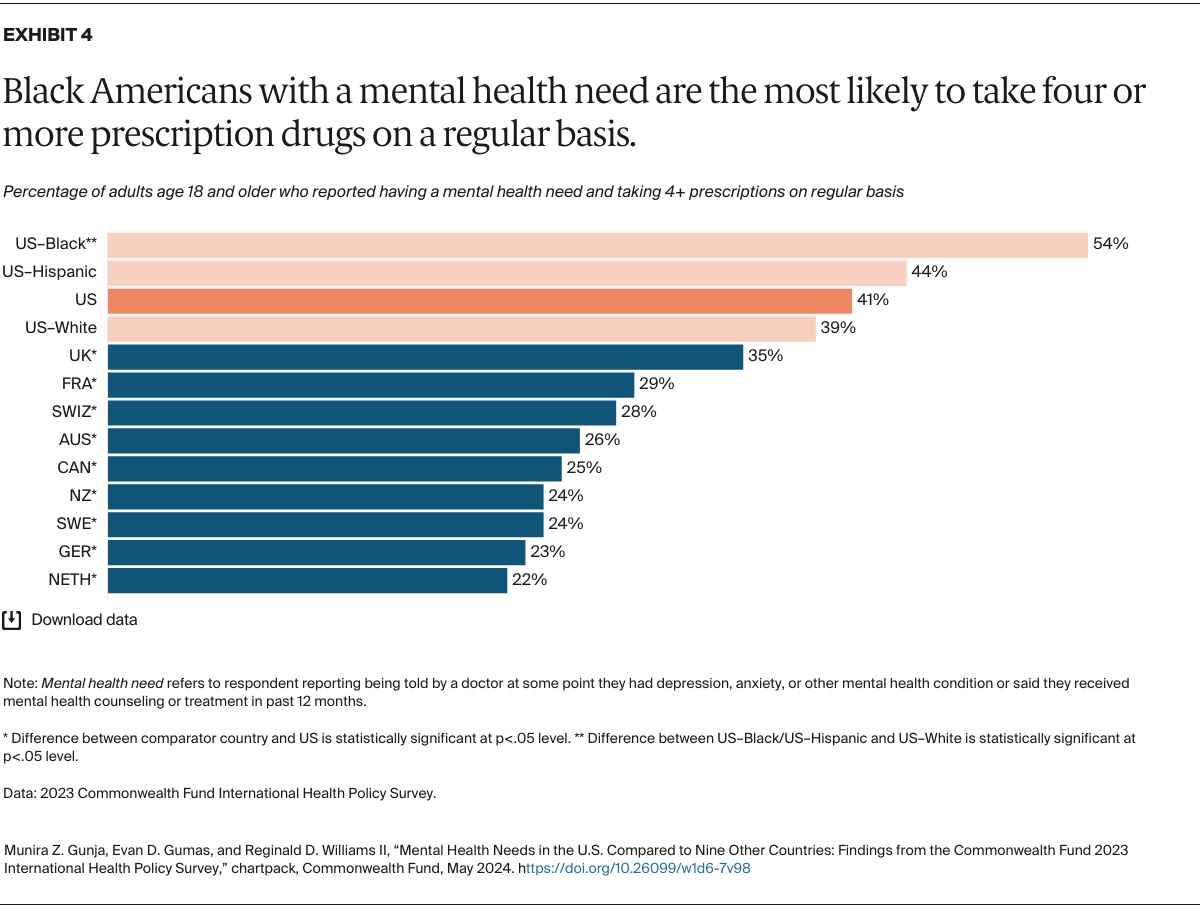
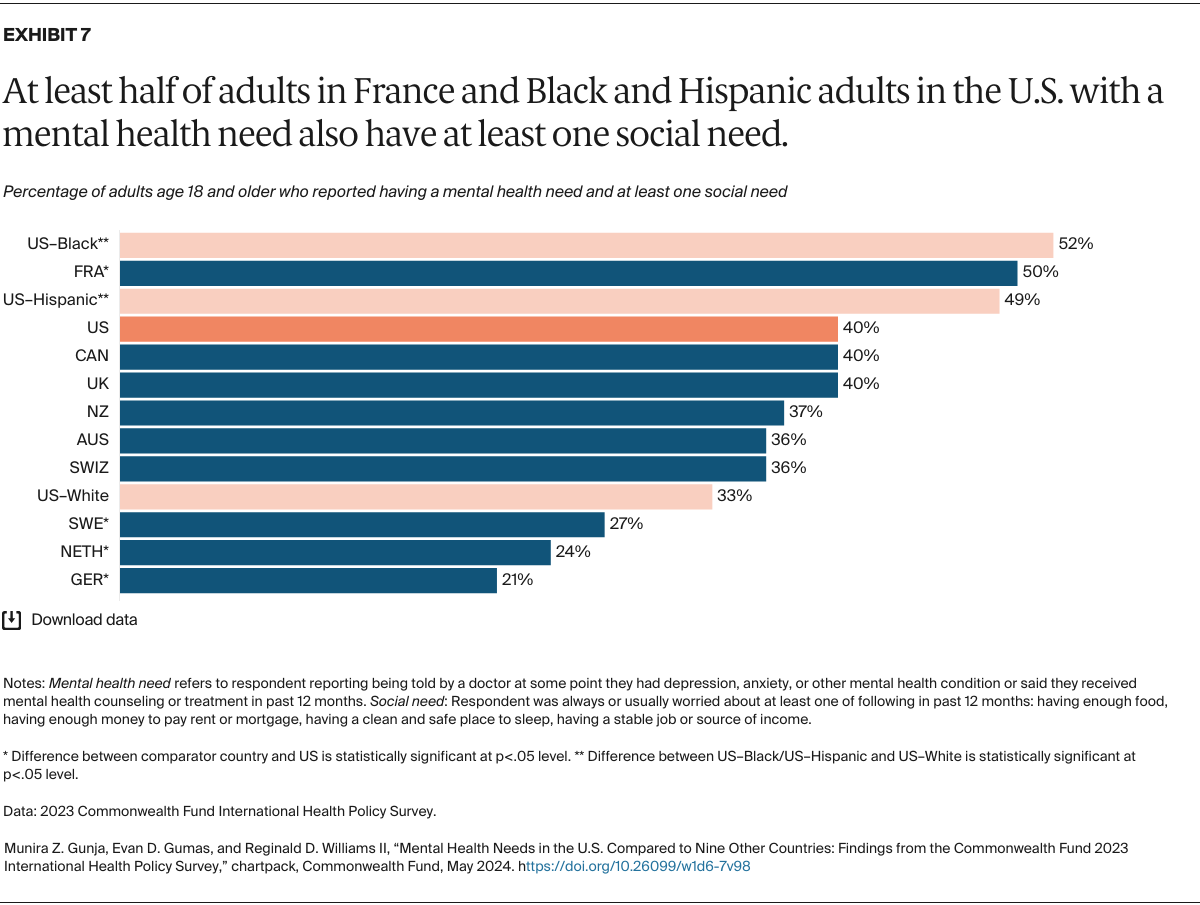
The consequences are severe. Mental health is deeply connected to physical health outcomes, as well as to social and economic well-being. People with behavioral health conditions are at greater risk of developing chronic conditions like heart disease or diabetes and more likely to lack secure housing, stable employment, and access to nutritious food.
In the U.S., more than half of all mental health spending and nearly three-quarters of substance use treatment funding come from public payers such as Medicare and Medicaid. While the Affordable Care Act has made significant strides in improving access to mental health care, work remains to ensure equitable access for all people.
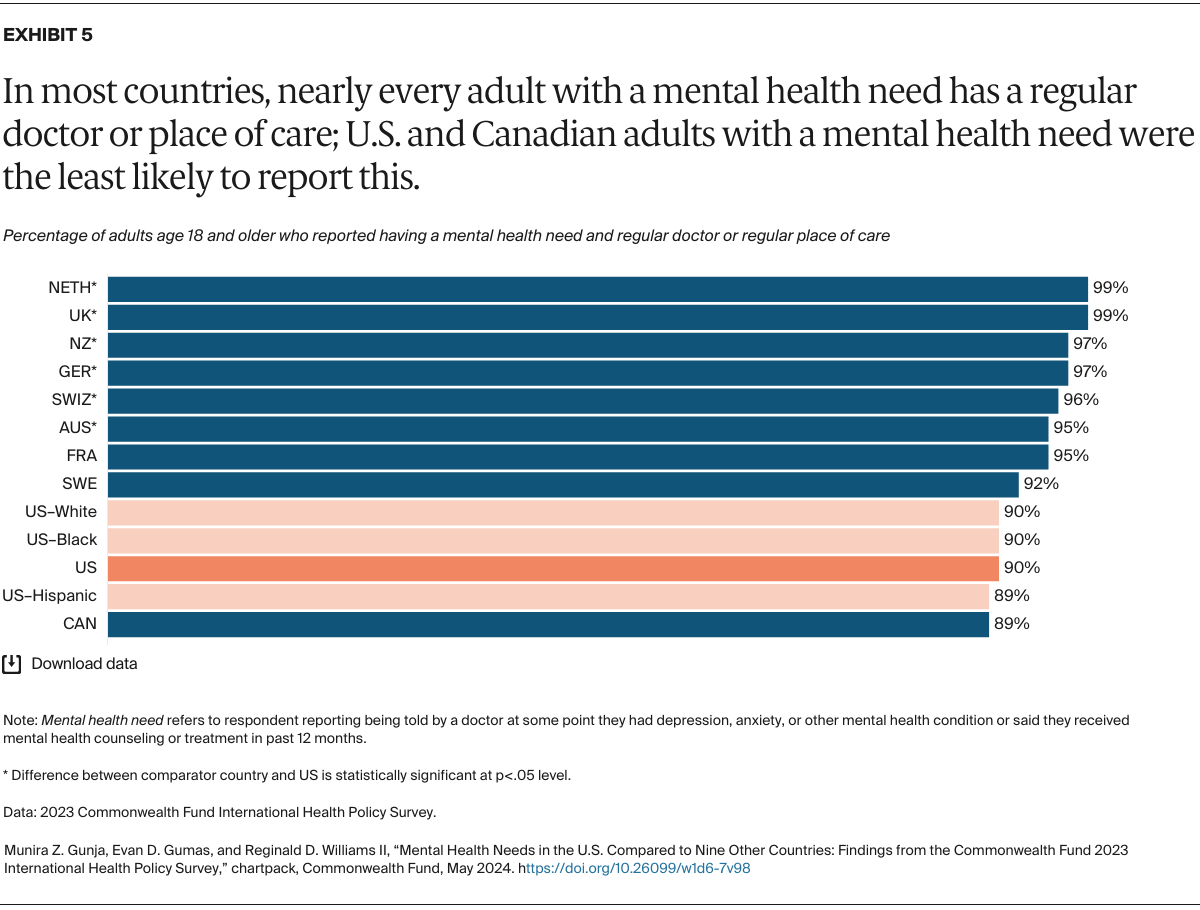
The following charts compare people’s mental health burden and ability to access and afford needed mental health care in the U.S. and other high-income countries. The data come from the 2023 Commonwealth Fund International Health Policy Survey of more than 21,000 adults age 18 and older in 10 countries. Findings on intentional self-harm were obtained from the Organisation for Economic Co-operation and Development (OECD).