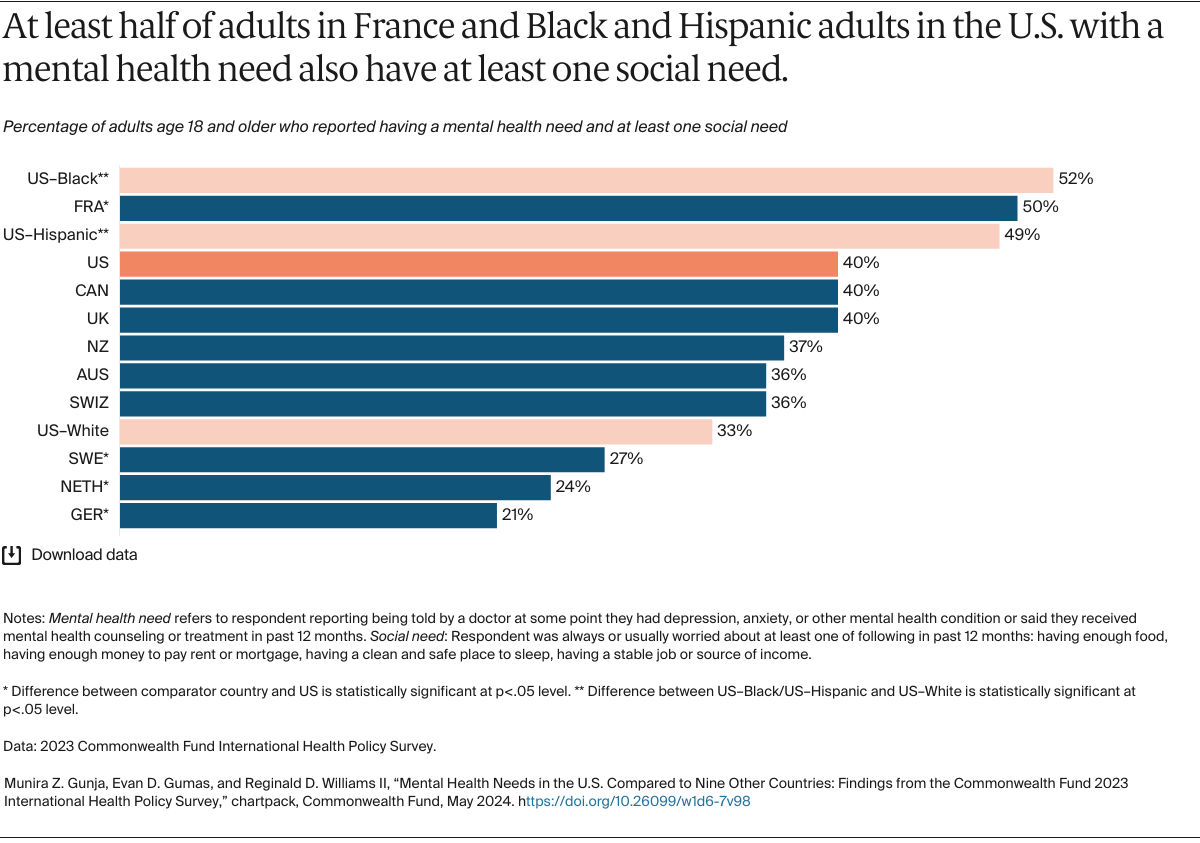
Nearly all countries are grappling with ways to improve social support for people with mental health needs. Half of Black and Hispanic adults in the U.S. and over half of all adults in France with mental health needs reported at least one social need, compared to only one of five adults in Germany.
While all countries have room to improve, some have had more success helping connect people with mental health needs to social support services. Doing so requires governments and institutions to strategically invest and allocate resources to social programs and interventions. This also means a shift in thinking that prioritizes mental health and social needs as part of health care. We can improve health by considering both physical and mental health in policy. Better living conditions — including housing and jobs — all impact a person’s total well-being.
What can we learn from countries that are addressing social needs and the impact on mental health?
Financial Security
People that report greater financial worries show more depressive and anxiety symptoms; policies that support financial security can protect and improve mental health. Fewer than 5 percent of adults in Germany and the Netherlands, regardless of income level, reported cost barriers to accessing mental health care. Germany offers generous income support, including for the unemployed, and also offers parental leave and highly subsidized early childhood education. Germany’s commitment to funding its aging populations stands out. The generous policy alleviates the burden for relatives to become caretakers, which allows them to focus on their own lives and responsibilities. Germany’s long-term care law covers most of the nation’s elderly.
In the Netherlands, the nation’s home-care provider, Buurtzorg Nederland, delivers high-quality care at a low cost using self-governing nurse teams. Buurtzorg’s nurses provide not only medical services that require nursing training but also many support services, including dressing, shopping, cleaning, and preparing meals, which alleviates the financial burden for their families to provide this care.
Food
Poor nutrition is a significant risk factor for mental health needs, contributing to depression, anxiety, and even cognitive decline. People with mental health needs often experience higher rates of food insecurity, meaning they struggle to access healthy and affordable food. Ensuring access to nutritious food for all people is a crucial step toward promoting overall well-being.
Australia’s Equally Well program aims to eliminate food insecurity by ensuring all people with mental health needs have access to affordable and nutritious food. Community-based food relief agencies offer food-insecure individuals healthy, nutritious meals delivered through food trucks, mobile markets, and school-based programs. The Equally Well initiative requires involvement from stakeholders at all levels, and also includes a partnership with New Zealand.
Housing
The Canadian At Home/Chez Soi study found that Housing First programs are effective in treating mental health needs while providing stable housing and reducing homelessness. Housing First programs provide permanent housing to people experiencing homelessness and then follow up with social support services after individuals are placed in housing. Housing First has been adapted in several countries around the world. While several cities in the U.S. have adopted the model, underinvestment in critical supports, like mental health and substance use care, as well as a lack of coordination between providers, has created barriers to successful implementation.
Jobs
In the United Kingdom, a study found that when people moved from unemployment or stay-at-home parenting into paid work (i.e., up to eight hours per week), their risk of mental health needs were reduced by an average of 30 percent. The U.K. launched a program, implemented by its Department of Work and Pensions, that provides a 20-hour, job-search-skills workshop for individuals struggling with finding employment. Research found that there were significantly lower rates of depression and anxiety among participants six months after completing the course.
While policymakers work to address mental health demands in their countries, our findings show that addressing the rate of mental health needs may only be successful if reforms are made to address other areas of health, including social drivers like food and housing insecurity. The current cycle of poverty, discrimination, and mental health requires a strategic response; the well-being of our countries depends on prioritizing mental health. Learning from successful approaches in other countries can provide valuable inspiration for addressing mental health and social drivers in the United States.