In 2021, Medicare Advantage (MA) plans denied 6 percent, or more than 2 million, prior authorization requests — that is, beneficiary requests for coverage of a specific service or treatment. An MA plan may determine that a service is not medically necessary, not a covered benefit, or that a more cost-effective service is available, among other reasons. When this happens, beneficiaries may file an internal appeal (referred to as a Level 1 appeal), requesting that the plan reconsider the denial decision. A report by the U.S. Department of Health and Human Services Office of the Inspector General found that between 2014 and 2016 only 1 percent of denials were appealed by enrollees. However, on appeal, the plan overturned 75 percent of the denials it reviewed — meaning the plan decided in favor of the beneficiary and agreed to provide coverage for the requested service.
Denials that are not overturned by the plan following Level 1 review are automatically submitted for Level 2 review, which is performed by an independent entity, known as the Medicare qualified independent contractor (QIC).1 Following review of the appeal, the QIC may determine that the MA plan appropriately denied coverage, and thereby uphold the plan’s denial. Alternatively, the QIC could determine that the plan erroneously denied coverage. In this event, the QIC would overturn the denial and require the plan to cover the service.
Coverage denials are troubling because they may lead to delays in obtaining needed care and potentially result in adverse health outcomes. In the interest of promoting timely access to care, the Centers for Medicare and Medicaid Services includes a measure that assesses plans on the number of Level 1 denials upheld by the QIC. This is part of the MA Star Ratings, which rate plans on quality of care and customer satisfaction.
There are limited publicly available data on trends in beneficiary appeals to MA plans (i.e., Level 1 appeals). However, the QIC routinely reports on the volume of Level 2 appeals and the extent to which the QIC either upholds or overturns MA plans’ decisions. Although these data only include appeals reviewed by the QIC, they do provide insight into the extent to which plans are able to interpret and apply coverage policies.
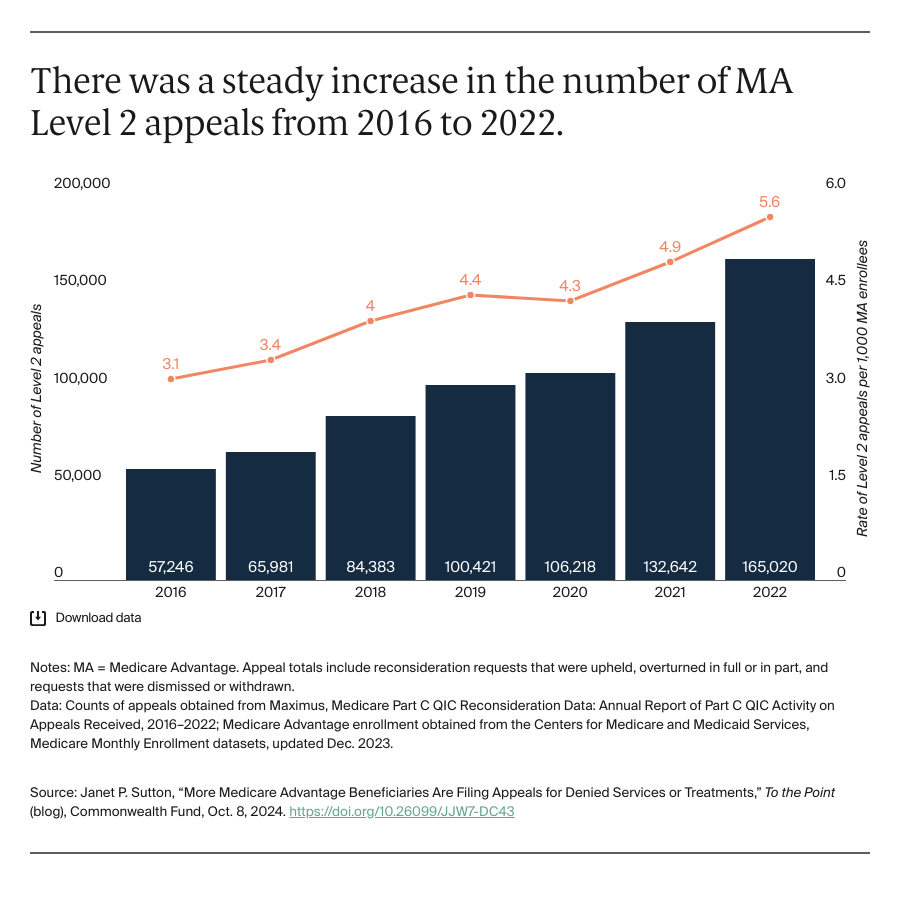
An Increase in the Volume of Appeals
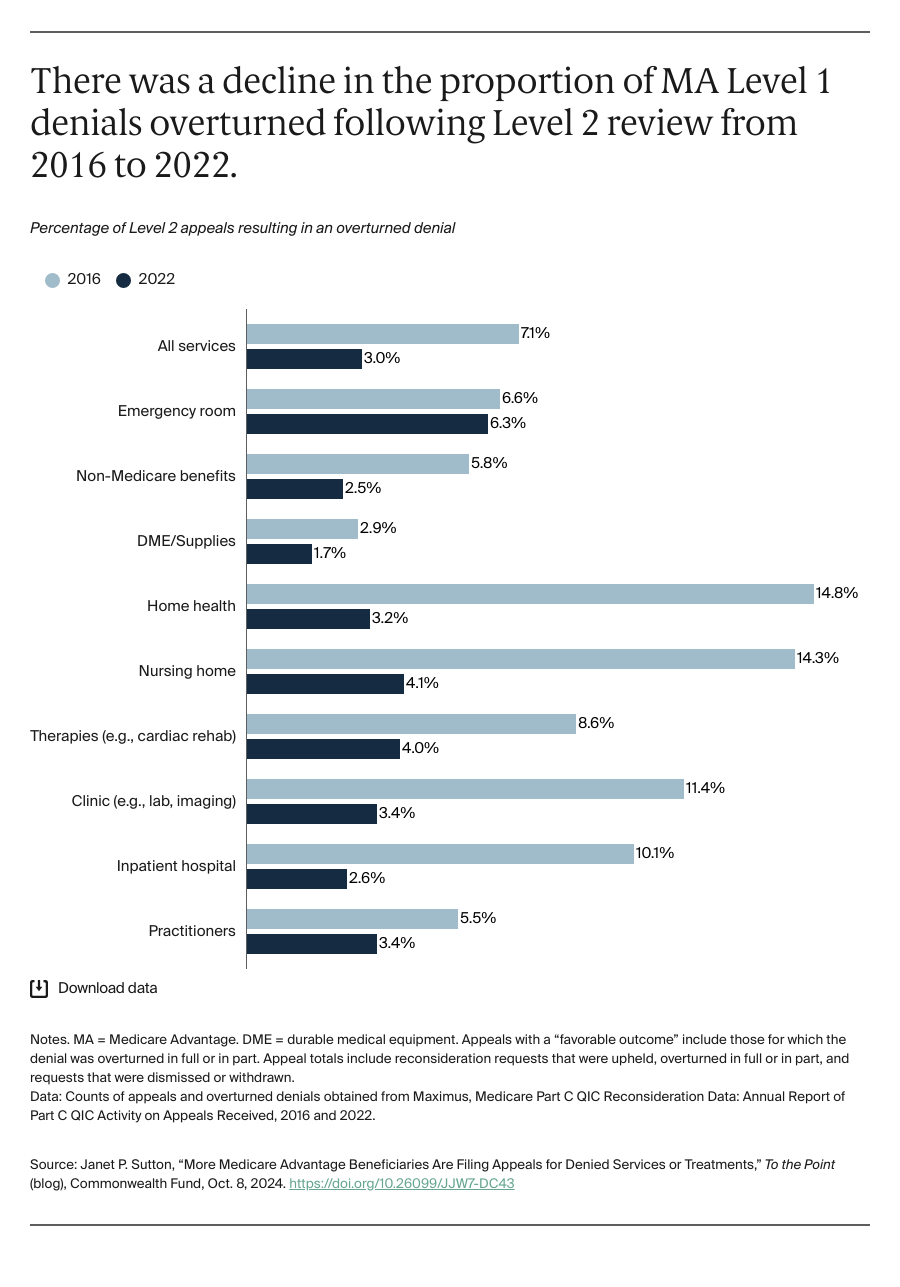
The QIC received 165,000 appeals in 2022, or 5.6 appeals per 1,000 MA enrollees. Almost two-thirds of these fell into three categories: practitioner services (e.g., physician office visits); non-Medicare/supplemental services (e.g., dental and vision care); and clinic services (e.g., laboratory tests, imaging). Overall, only 3 percent of Level 2 appeals resulted in a favorable coverage determination — an overturned denial — for the beneficiary. The service category with the highest proportion of overturned denials was emergency room visits, for which the QIC overturned 6.3 percent of Level 1 denials. Other categories with high overturn rates included nursing home services, and therapies (e.g., physical therapy and cardiac rehabilitation); both service categories had overturn rates of approximately 4.0 percent. The lowest overturn rate was for durable medical equipment (1.7%).