There is an ongoing behavioral health crisis in the United States. Behavioral health care is costly, difficult to access, and not equitably provided. These challenges cannot be addressed with the behavioral health specialty care workforce alone, owing to insufficient number of providers, particularly in rural areas. To equitably meet the needs of people with mental health and substance use disorders, behavioral health care must be integrated with primary care to ensure that people get access to effective care quickly and in an accessible and trusted setting.
A New Approach to Primary Care
Recently, the Center for Medicare and Medicaid Innovation (CMMI) took an important step toward supporting high-quality primary care by launching Making Care Primary (MCP), a model that focuses on bringing more providers into value-based payment arrangements and supporting behavioral health integration. Using a tiered payment approach, CMMI has laid out incremental steps to enable providers unfamiliar with value-based payments to build infrastructure and gain experience with risk sharing. The model also presents an opportunity to scale and spread behavioral health integration.
Solving Key Challenges in Behavioral Health
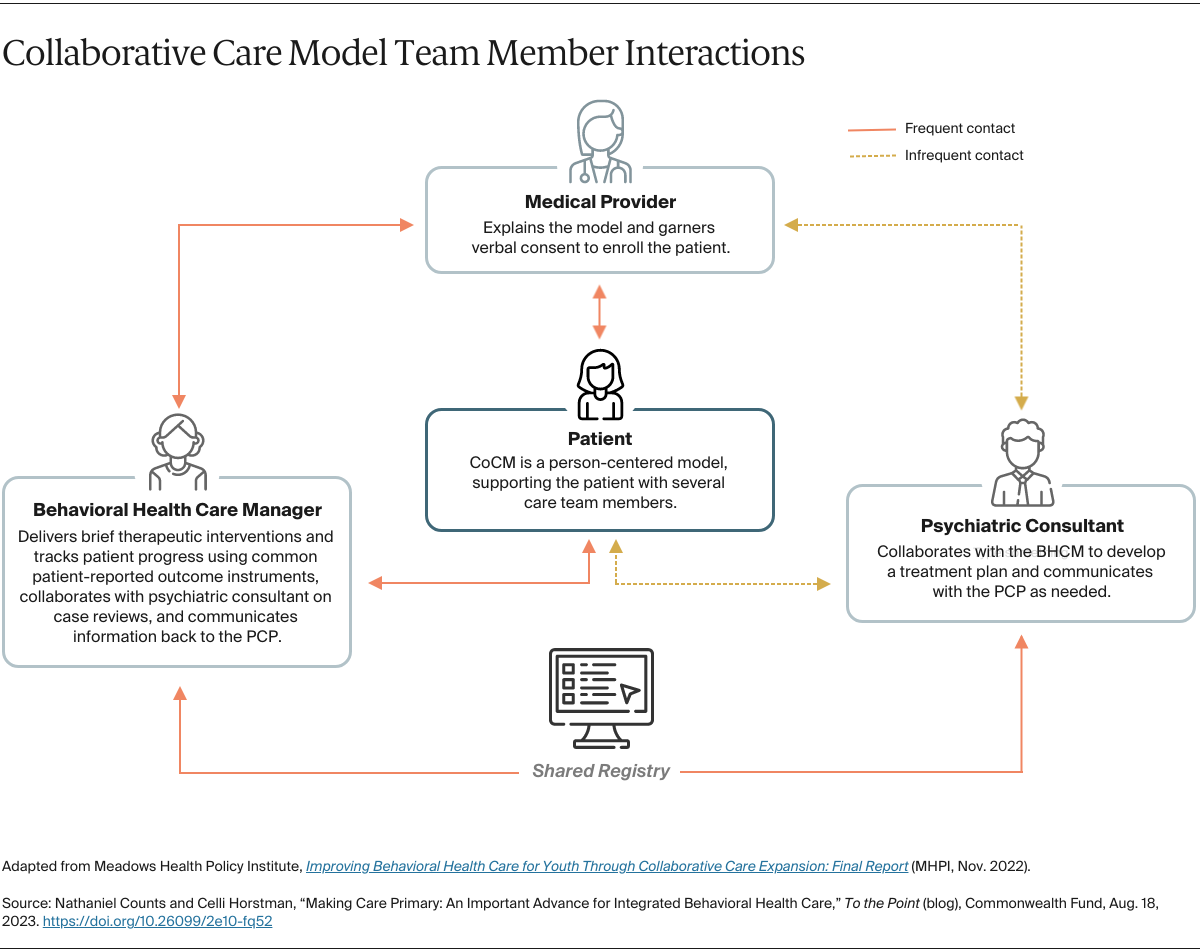
Primary care integration expands access to behavioral health care by treating patients where they are already seeking care — that is, their primary physicians’ offices. In one evidence-based approach, the Collaborative Care Model, primary care providers identify and treat behavioral health needs with the support of a consulting behavioral health specialist and a care manager. As a team, they provide short-course psychotherapy, prescribe medications as appropriate, track progress of symptoms, and refer patients to higher levels of care as needed.