The COVID-19 pandemic is at a crossroads in the United States. On the one hand, U.S. cases, hospitalizations, and deaths have trended dramatically downward from their peaks in January 2022. Many jurisdictions have relaxed their pandemic restrictions, and many people have returned to in-person work and social events, creating a sense that the end is near. On the other hand, hundreds of deaths are still reported each day, and cases have again started to rise in several parts of the U.S. as the highly contagious Omicron subvariant BA.2 has taken hold as the dominant virus variant. In coming weeks, COVID-19 outbreaks in Europe and China may foreshadow another surge in U.S. cases.
Amid this uncertainty, Congress is debating the need for additional pandemic-related policies. Federal funding for testing and coverage of vaccination costs is poised to expire as the public health emergency ends. Some are questioning the need for vaccines and boosters. But others are warning about the potential impact of waning immunity and new variants driving outbreaks even among previously vaccinated groups.
In December 2021, we reported that the first year of the U.S. vaccination effort had averted 1.1 million deaths and 10.3 million hospitalizations (compared to a no-vaccine scenario), primarily by blunting a surge in the Delta variant during the summer and early autumn of 2021. Since then, nearly all U.S. regions have experienced a massive wave of infections, hospitalizations, and deaths caused by the highly transmissible Omicron variant. Yet that wave could have been much larger in the absence of a vaccination program. As Congress considers whether to fund additional vaccination programs, two pressing questions are: What was the impact of U.S. vaccination efforts on this most recent outbreak? And how much spending on health care was avoided?
In this post, we update our estimates to include the winter Omicron wave, calculating the numbers of COVID-related deaths and hospitalizations avoided because of the U.S. vaccination program. Additionally, we estimate in U.S. dollars the health care spending averted as a result of COVID-19 vaccination. To do so, we used a model that encapsulates the characteristics of the coronavirus variants, their transmission, and outcomes to compare the observed pandemic trajectory (of infections, hospitalizations, and deaths) to a counterfactual scenario in which no vaccination program existed. The model accounts for waning immunity and changes in population behavior over time as schools and businesses have reopened and travel has increased. We have refined our model to reflect emerging scientific evidence. See “How We Conducted This Study” for further details.
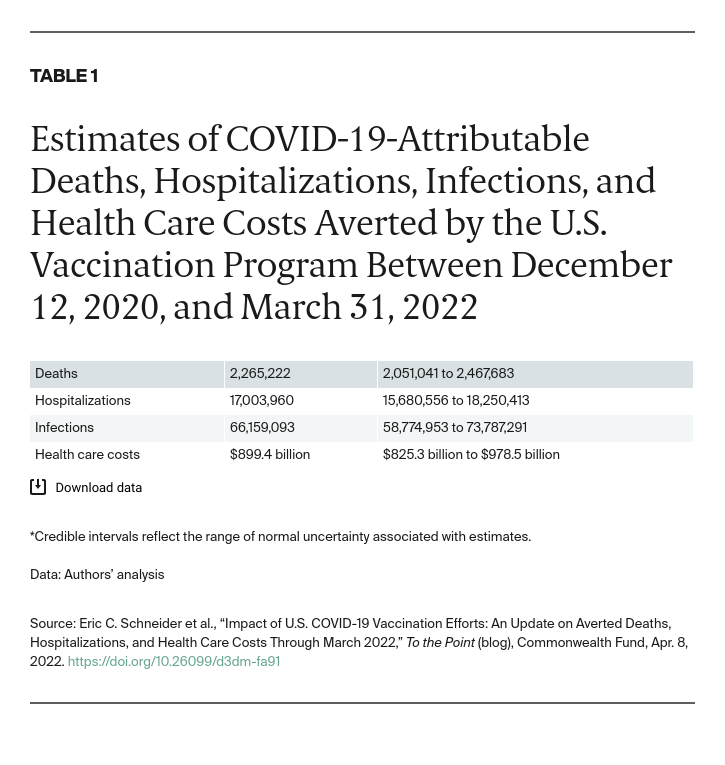
Through March 2022, we estimate that COVID-19 vaccination efforts in the U.S. prevented over 2 million deaths and 17 million hospitalizations (Table 1). There would have been an estimated 66 million additional infections and nearly $900 billion in associated health care costs in the absence of vaccination.
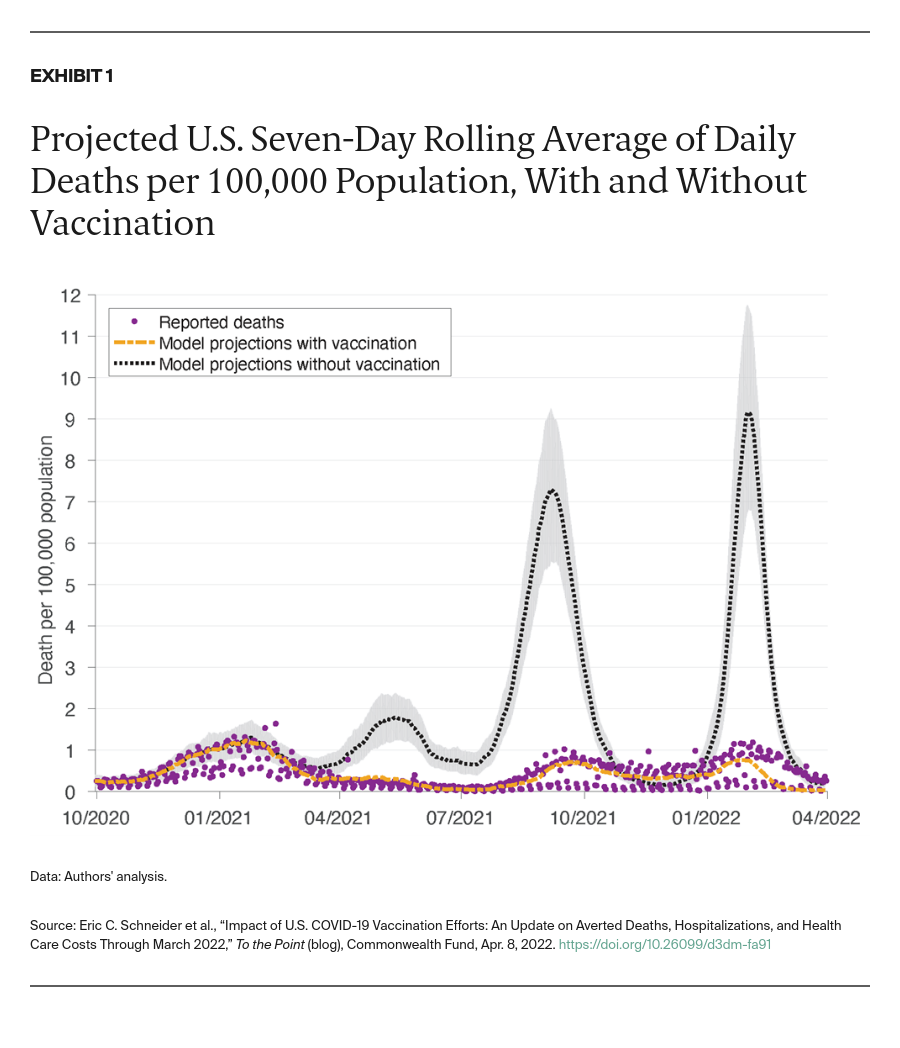
As Exhibit 1 illustrates, the daily peak of deaths pre-Omicron without vaccination would have exceeded 24,000 per day (7.3 per 100,000 population), far eclipsing the actual peak of 4,300 per day (1.3 per 100,000 population) reached during winter 2021.
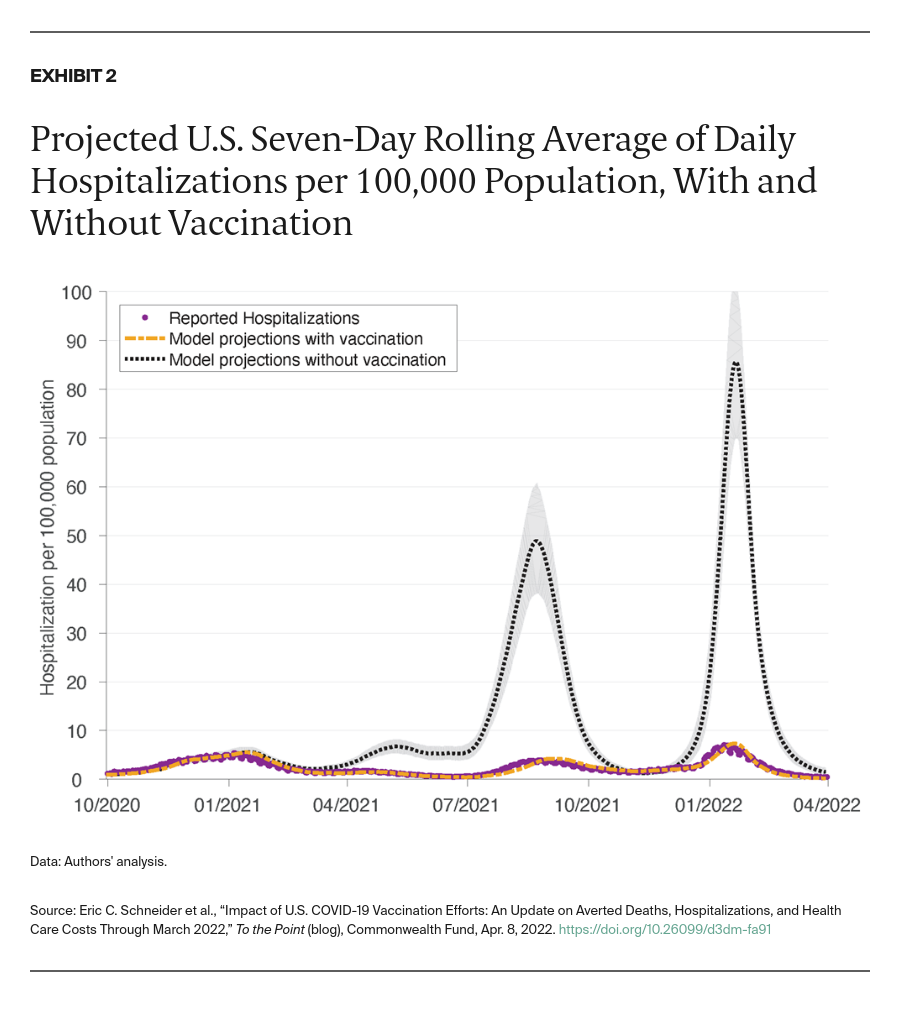
Exhibit 2 shows a similar pattern for hospitalizations without vaccination. During the Delta wave, hospitalizations would have peaked at more than 48 per 100,000 population; during the Omicron wave, they would have peaked at 85 per 100,000 population, exceeding the hospitalization rate attributable to influenza during an entire severe flu season.
The Continuing Urgency of Vaccination Efforts and Need for Ongoing Funding
Our findings highlight the profound and ongoing impact of the vaccination program in reducing infections, hospitalizations, and deaths. As we noted in our December analysis, vaccines spared the U.S. health care system an overwhelming number of COVID-19 hospitalizations. The current analysis confirms and extends the earlier results. Investing in vaccination programs also has produced substantial cost savings — approximately the size of one-fifth of annual national health expenditures — by dramatically reducing the amount spent on COVID-19 hospitalizations. Our analysis focused on avoided health spending does not include other savings related to continued productivity at work and avoided loss of lives.
The success of the vaccination program in preventing deaths and hospitalizations is obscured somewhat by the nearly 1 million COVID-19 deaths that have occurred since the start of the pandemic. As Congress considers the costs and benefits of extending COVID-19 vaccination, our results show that continuing to vaccinate and boost Americans can produce substantial health benefits and financial returns to the country. Unvaccinated Americans have rates of preventable COVID-19 hospitalization and death that are significantly higher than those for vaccinated Americans.
In late March, the Centers for Disease Control and Prevention recommended a second booster for certain immunocompromised individuals and people over age 50. Yet only about a third of eligible adults have received their first booster shots. Daily vaccination rates are at their lowest rate since the beginning of 2021. As immunity wanes, breakthroughs and second infections will invariably rise. In January, we estimated that doubling or tripling the daily booster vaccination rate could avert tens of thousands of deaths and hundreds of thousands of hospitalizations during the Omicron wave.
Redoubling efforts to increase vaccine uptake, especially among the elderly and other vulnerable groups, will be critical to avert outbreaks as pandemic restrictions are lifted. With continued spread of the BA.2 subvariant, our findings point to the tremendous power of vaccination to reduce disease burden from COVID-19. This may be even more important if newer variants arise or population immunity ebbs. Without continued funding, the lifesaving impact of vaccinations are at risk.