Abstract
- Issue: During the past 14 years, the federal government and states have fielded numerous value-based payment (VBP) models for primary care to move away from a fee-for-service payment model that incentivizes the delivery of more services over better-quality care. However, most primary care practitioners (PCPs) do not participate in VBP models, and the reasons are largely unknown.
- Goals: Learn the barriers PCPs face to participating in VBP models from those who have not joined them and identify potential solutions.
- Methods: Interviews with 12 PCPs in leadership positions and other primary care management experts and focus groups with 17 frontline PCPs with no prior participation in VBP primary care models.
- Key Findings and Conclusion: PCPs’ enthusiasm for VBP models is tempered by financial barriers, the PCP workforce shortage, and imperfect performance measures. Suggested solutions to the financial challenges include sufficient upfront primary care payments from the models and ensuring health systems transfer the value-based payments to frontline primary care practices. Solutions to the PCP workforce shortage include increasing payments, boosting supports for PCPs, and investing in primary care trainees. PCPs felt that current performance measures could be improved by swapping out condition-specific metrics for metrics that support access and continuity of primary care.
Introduction
The Centers for Medicare and Medicaid Services (CMS) and a number of states have introduced value-based payment (VBP) models focused on primary care since 2010. These models aim to incorporate more upfront and results-based payments to move primary care practitioners (PCPs) off the “hamster wheel” of fee-for-service payments that incentivize them to deliver higher volumes of services.1 VBP models build on patient-centered medical home efforts2 and share similar goals, such as strengthening the primary care infrastructure and improving patients’ access to high-quality care, to ultimately improve health outcomes and reduce unnecessary health care spending.3 Several VBP models encourage collaboration across public and commercial payers to reduce reporting burden and incentivize care improvement by ensuring they include a high proportion of a PCP’s patients.
Despite the potential of these models to strengthen the primary care infrastructure and improve patient care,4 most primary care practices do not participate in them. A 2022 survey found that just 46 percent of primary care physicians reported receiving any value-based payments.5 The smaller, independent, and less-resourced practices that serve 39 percent of traditional Medicare beneficiaries are the least likely to apply to VBP models; their lower participation rates mean communities with fewer economic resources may not be seeing the benefits of increased primary care investment.6 Why certain PCPs never take part in VBP models is largely unknown, as most information collected on the topic comes from practitioners already participating in models.
For this study, we spoke directly to PCPs without VBP model experience to understand why they do not participate. Our findings come from focus groups and key informant interviews with 29 respondents. Focus group respondents included frontline PCPs in family medicine or general internal medicine who had never participated in state or federal VBP primary care models. However, a few worked at organizations that participated in accountable care organizations (ACOs), a type of VBP model that allows providers to work together to coordinate care and potentially share in any savings that result.7 Key informant interviewees (which we will refer to as experts) included PCPs and individuals from primary care member associations that interact with and support frontline PCPs. (See “How We Conducted This Study” for further detail.)
Findings from this study can show policymakers how to make VBP models more attractive to PCPs, especially those from practices with fewer resources. Robust participation will be critical to evaluating a payment approach that can strengthen primary care — the backbone of an efficient, high-quality, and equitable health care system.
Study Findings
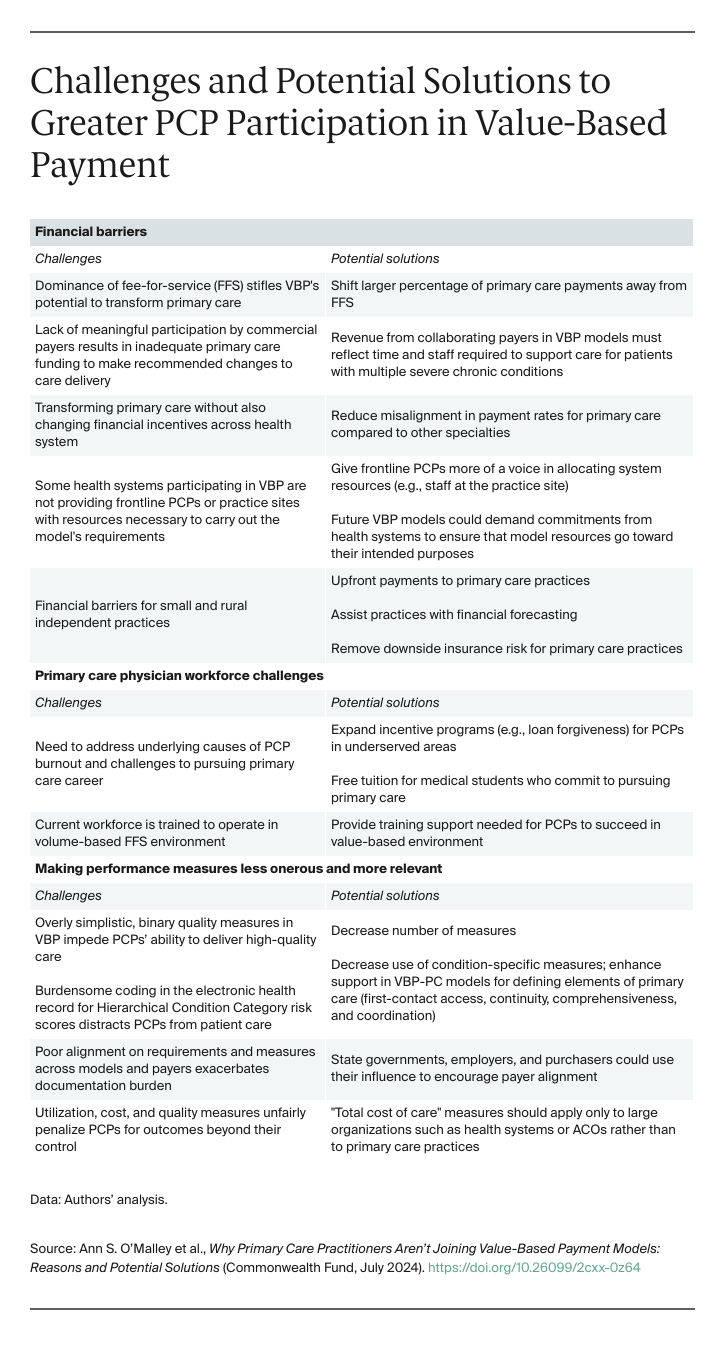
Overcoming Financial Barriers to Participating in VBP Models
The current dominance of fee-for-service (FFS) stifles VBP models’ potential to transform primary care delivery. Participants noted that most primary care revenue is still FFS, even for PCPs participating in VBP models. Decreasing PCPs’ reliance on distorted FFS payments would help reduce the pressure to maximize visits per day and instead allow primary care practices to focus on the models’ goals of proactively managing patient populations and providing timely care that responds to patients’ needs and preferences. One expert said getting PCP buy-in for VBP models has been difficult because “it’s just [FFS] with this extra layer of reporting and accountability that the system is not structured to support.”
Lack of meaningful participation by commercial payers in VBP models results in inadequate primary care funding to make the recommended changes to care delivery. Even though several VBP models encourage collaboration between commercial and public payers, experts noted that most commercial payers have not sufficiently engaged in them, and those that have have chosen to make relatively small enhanced primary care payments. Furthermore, commercial payers have shifted little of their payments in these models away from FFS. As a result, practices receive insufficient increases in primary care revenue, which limits their ability to change care delivery. Participants noted that revenue from collaborating payers in VBP models must reflect the time and staff required to support care for complex patients and those with multiple severe chronic conditions. This includes hiring staff such as community health workers and nurses to help with advanced access, between-visit care management, care coordination, screening, and linking patients to supports for their health-related social needs.
For system-affiliated practices, it’s a challenge to transform primary care without also changing financial incentives across the health system. Many VBP model participants are part of large health systems that include hospitals and specialty care.8 Without changing incentives for specialty and hospital-based services, health systems have little reason to meaningfully invest in disease prevention and maintenance by changing primary care delivery. That’s because primary care cognitive services are poorly compensated compared to more procedurally oriented specialty services.9 In fact, PCPs and experts noted that many health systems see VBP models as an avenue to increase referrals to their more lucrative specialty and hospital facility services rather than improve primary care delivery.
Some health systems participating in VBP models are not providing frontline PCPs or practice sites with the resources necessary to carry out the model requirements. One expert said health systems are “using their contracting authority to [join a model] on behalf of those doctors but not reliably transmitting those resources to the primary care practice.” For example, two PCPs said that, when they asked for more nurses at the practice sites, the health system hired a nurse but seated her at the corporate office. An expert who works with primary care practices across health systems said system-owned practices that do well in VBP models transfer resources to support care delivery changes at the practice sites. Focus group participants suggested that frontline PCPs should have a voice in allocating system resources, including the types of staff needed at their practice sites. Another expert suggested that future VBP models should demand commitments from health systems to ensure that model resources go toward their intended purposes.
Small and rural independent practices face further financial challenges to participating in VBP models. Small or rural independent practices generally have fewer financial resources and narrower profit margins than larger, system-affiliated practices, and slight changes in revenue can threaten their financial viability. And because they see fewer patients than larger practices do, small independent practices typically receive less revenue from VBP models. The smaller total payments, combined with more limited financial reserves, mean independent practices might not be able to cover the cost of resources needed to enhance care delivery, such as adding staff or upgrading health information technology.
To help manage the financial risk of participating in VBP models, practices would benefit from upfront payments, assistance with financial forecasting, and removing downside insurance risk. Participants said VBP models do not need to expose PCPs to potential financial losses or penalties (that is, downside risk). They felt that independent practices need more information about how model participation would affect their revenues during each year of the model. Upfront payments at the start of model participation would help practices with limited financial reserves invest in resources to improve care delivery and participate in the models.
Addressing Primary Care Workforce Challenges That Thwart VBP Model Participation
VBP models would be more attractive if the underlying primary care workforce shortage could be addressed. While a goal of the models is to help address the shortage and alleviate physician burnout, that has not been achieved to date.
Primary care physicians are critical to the workforce because of their extensive training in managing complex patients with multiple chronic conditions. But the workforce shortage has left many physicians overwhelmed with large patient panels, stress that is compounded by heavy administrative burdens and inadequate supports. Facing an average $200,000 in medical school debt, new doctors often pursue more lucrative medical careers as hospitalists or subspecialists.10 Other PCPs avoid billing hassles by working in the direct primary care model or concierge practices.11 Participants said enrolling in a VBP model that some see as increasing their work without reducing their challenges feels overwhelming. Any VBP model seeking PCPs’ engagement will be more successful if it responds to these underlying challenges. An obvious solution is to increase payments to primary care, but participants said this needs to be accompanied by supports to improve job satisfaction.
Payers and policymakers can consider additional ways to make primary care more attractive. PCPs suggested more incentives for physicians to join the primary care workforce. This includes expanding some incentive programs, such as loan forgiveness for primary care physicians who work in rural or other underserved areas and free tuition for medical students who commit to pursuing primary care.
Payers and policymakers should consider the training support needed for the primary care workforce to succeed in the value-based environment. Experts said the current workforce is trained to operate in a volume-based FFS environment. Shifting to proactive value-based care requires some instruction on panel management for existing PCPs, their staff, and medical trainees.
Making Performance Measures Less Onerous and More Relevant to Primary Care
PCPs worry that current quality measures used in VBP models impede their ability to deliver high-quality care. Value-based payment models tie the amount health care practitioners earn for their services to the results they deliver for their patients as measured in part by quality measures.12 PCPs in the focus groups felt that current measures that focus on binary or stark cut-offs for individual conditions or screening tests are overly simplistic and often fail to capture high-quality primary care. For example, one PCP described receiving a message from her health system asking her to talk to a patient about body mass index. But during a visit, the PCP observed that the patient was severely depressed; clearly, discussing the topic in that moment would have been insensitive.
PCPs are concerned about burdensome coding in the electronic health record for Hierarchical Condition Category (HCC) risk scores, saying it takes PCPs’ attention away from interacting with patients. Speaking of their experience with Medicare Advantage and, in a few cases, with ACOs, participants said health plans and health care systems encourage maximizing the diagnoses listed in the electronic health record to increase patients’ HCC risk scores. PCPs said time spent on burdensome HCC coding distracts from patient care. They felt that this documentation enhances payments to health plans and health systems rather than informing patient care.
Documentation burden is exacerbated by lack of alignment across models and payers. PCPs described how models and payers use different metrics, resulting in PCPs spending more time “meeting the requirements of insurers than meeting needs of patients.” Experts we interviewed thought that state governments, employers, and purchasers could use their influence to encourage payer alignment on measures and other reporting requirements.
PCPs have concerns about utilization, cost, and quality measures that they believe unfairly penalize them for outcomes beyond their control. For example, acute hospitalization rates and total Medicare expenditures are common measures of outcomes in VBP models but are mostly affected by patients’ other providers such as specialists and hospitalists.13 PCPs said quality measures might also penalize PCPs for patient- or societal-level factors such as patients’ preference to not receive a service or treatment, social needs that impede patients’ receipt of recommended services, or the accessibility and availability of other health care services in a patient’s neighborhood. To alleviate some of the pressures on PCPs, a few experts suggested that total cost of care measures should apply only to large organizations such as health systems or ACOs rather than to primary care practices.
Measures related to access, continuity, and communication might better reflect high-quality, patient-centered care. PCPs felt that measures of primary care access like appointment availability for same- or next-day visits, wait times, and contacts with patients between visits not only reflect good care but are also within their control. They also cited measures of continuous care, such as whether patients can see the same PCP at most office visits, and measures of communication, such as whether patients thought their PCP clearly explained how to prevent or manage diseases and treatment options.
Emphasizing Elements of Primary Care That Matter
Models should more heavily emphasize first-contact access, continuity, comprehensiveness, and coordination as “the foundation on which a health care system should be based.”14 Participants said shorter waiting times for primary care appointments and same-day visits could enhance access. They emphasized the importance of every person having a continuous relationship with a PCP, and the benefit of that relationship to patients, PCPs, and teams. PCPs wanted more time during visits to comprehensively address patients’ range of needs. They also wanted models to enhance care coordination with specialists through supports for improved communication via e-consults, more robust data exchange, and the ability to refer to a specialist outside one’s health system.
Given the high comorbidity of physical and mental health needs, PCPs and experts value the emphasis on behavioral health integration in recent VBP models. According to one PCP, “an integrated mental health program is priority number one . . . . [T]here’s no way you can succeed in a value-based care world if you can’t manage mental health issues in an efficient and coordinated way.”
Models centered around small care teams, with members embedded in the practice, are preferred. PCPs felt that teams of about three people are ideal: usually a PCP; a nurse or medical assistant; and another staff member who can help patients meet their needs, such as an embedded care manager, health coach, social worker, or community health worker. Large teams, according to some focus group members, lead to fragmented care and less accountability for meeting patients’ needs.