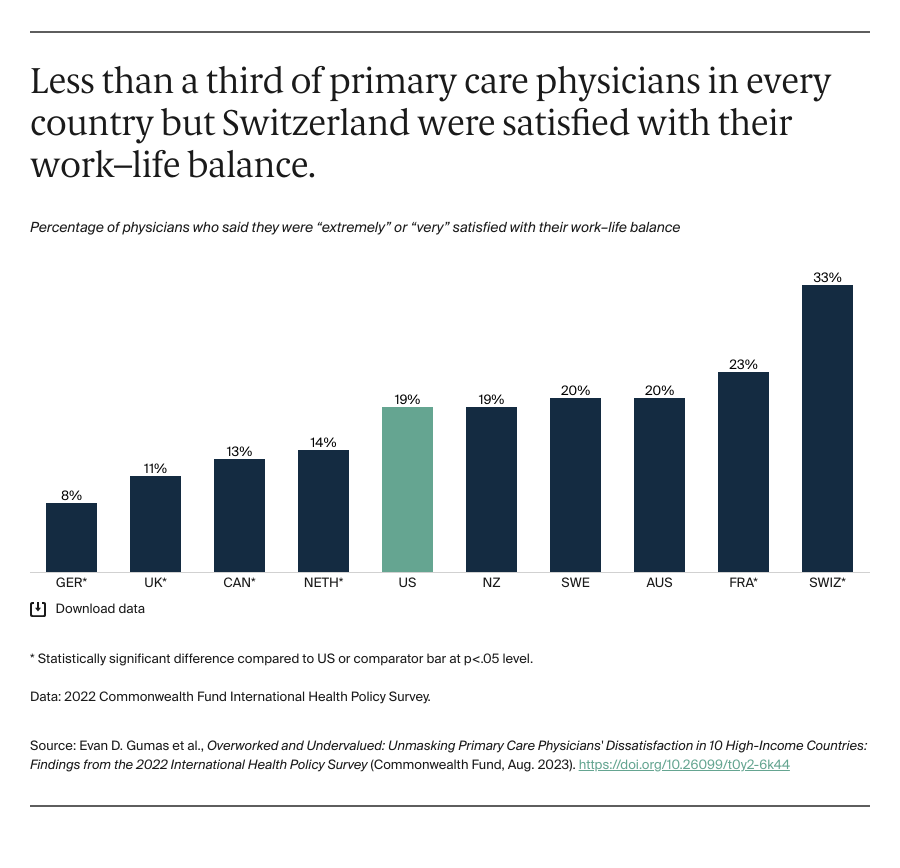
Apart from Switzerland, more than two-thirds of primary care physicians in every country said they were dissatisfied with their work–life balance. Only one of five physicians in the U.S. reported being satisfied. Research shows that maintaining a balanced life outside work — including getting proper sleep, nutrition, and exercise, and spending time with family and friends — is important for working efficiently and delivering consistently high-quality care to patients.6
Discussion
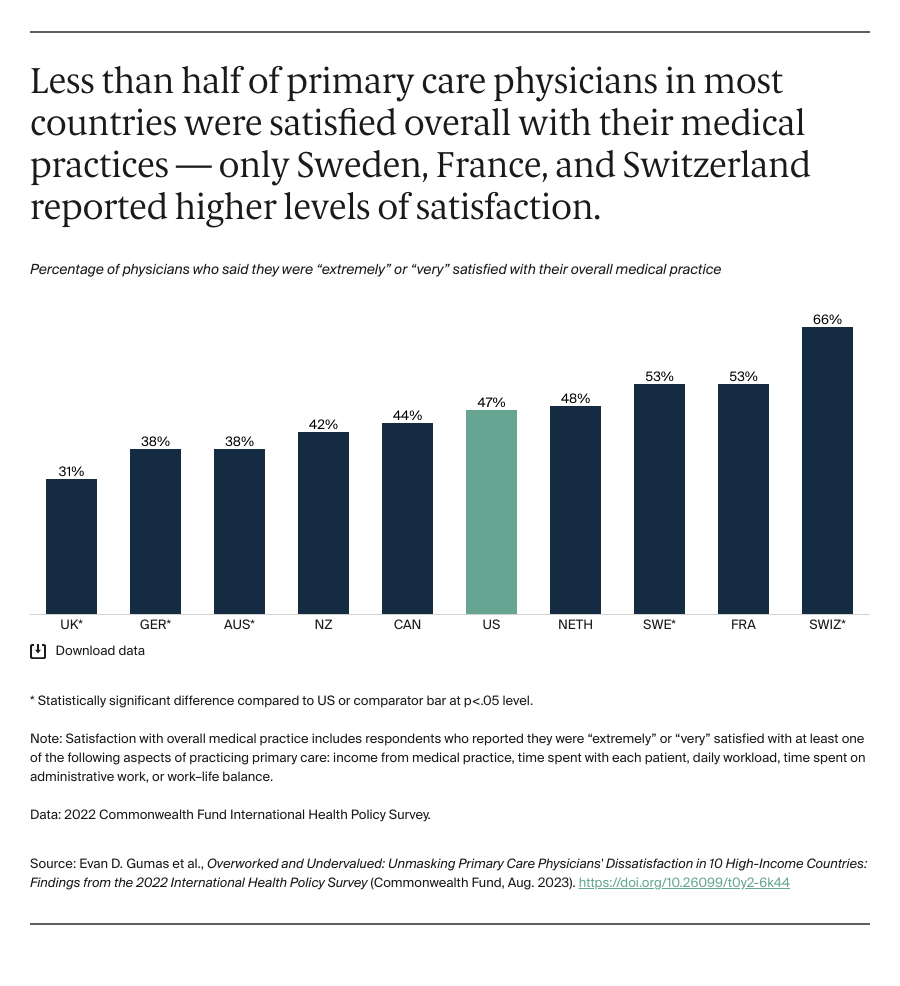
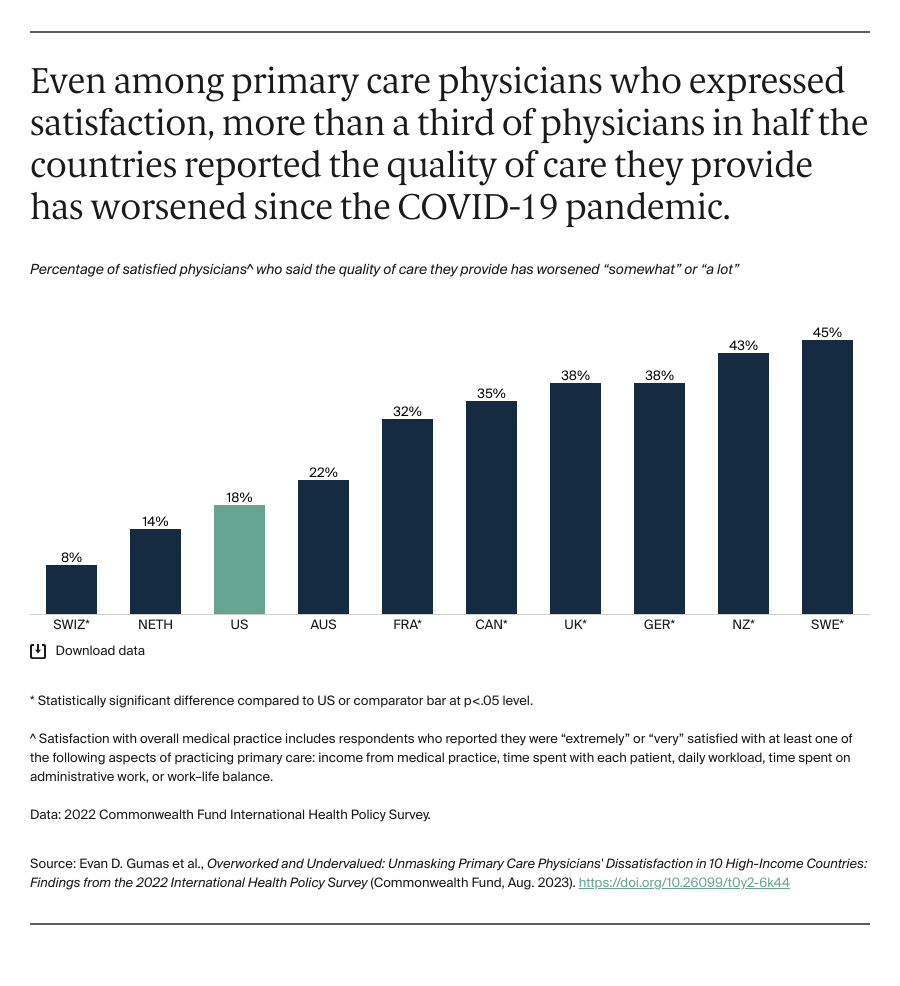
Our findings show that primary care physicians in all 10 countries are largely unsatisfied with several aspects of their medical practice. Even among physicians who reported feeling “extremely” or “very” satisfied, more than a third in half the surveyed countries reported the quality of care they were able to provide worsened with the COVID-19 pandemic. Evidence suggests satisfaction rates may vary within countries by practice size and location, with physicians in smaller or group practices being more satisfied than their counterparts in larger practices (sample-size limitations, however, prevented us from disaggregating our analysis).7
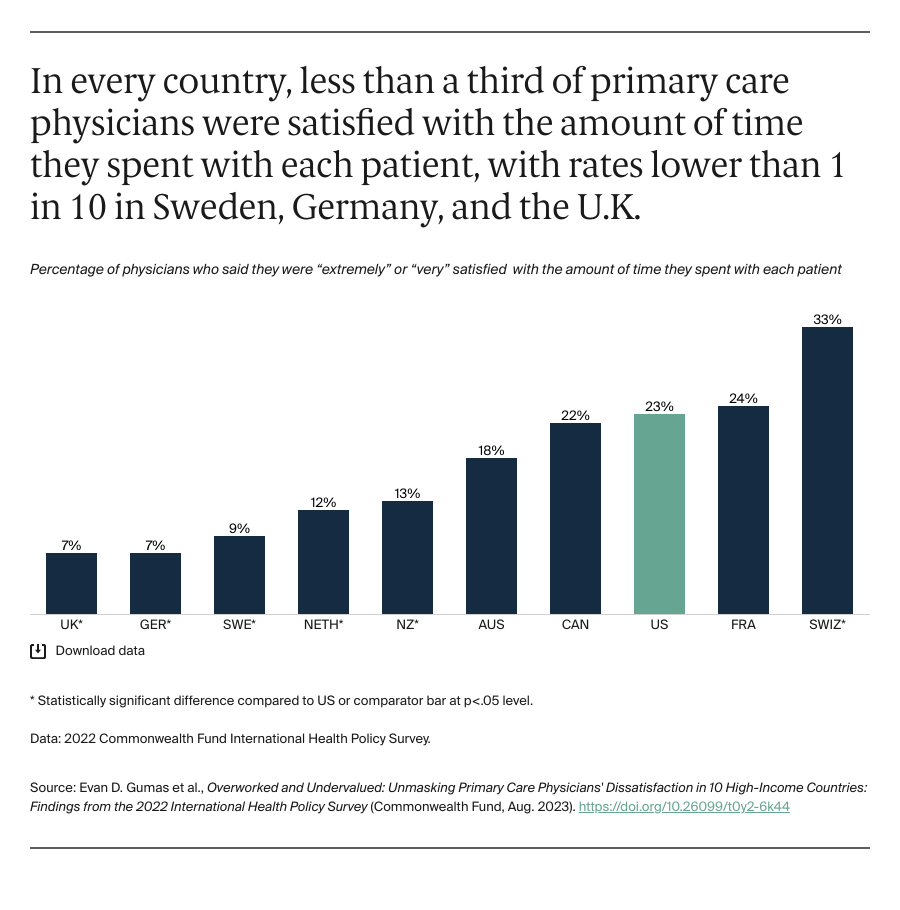
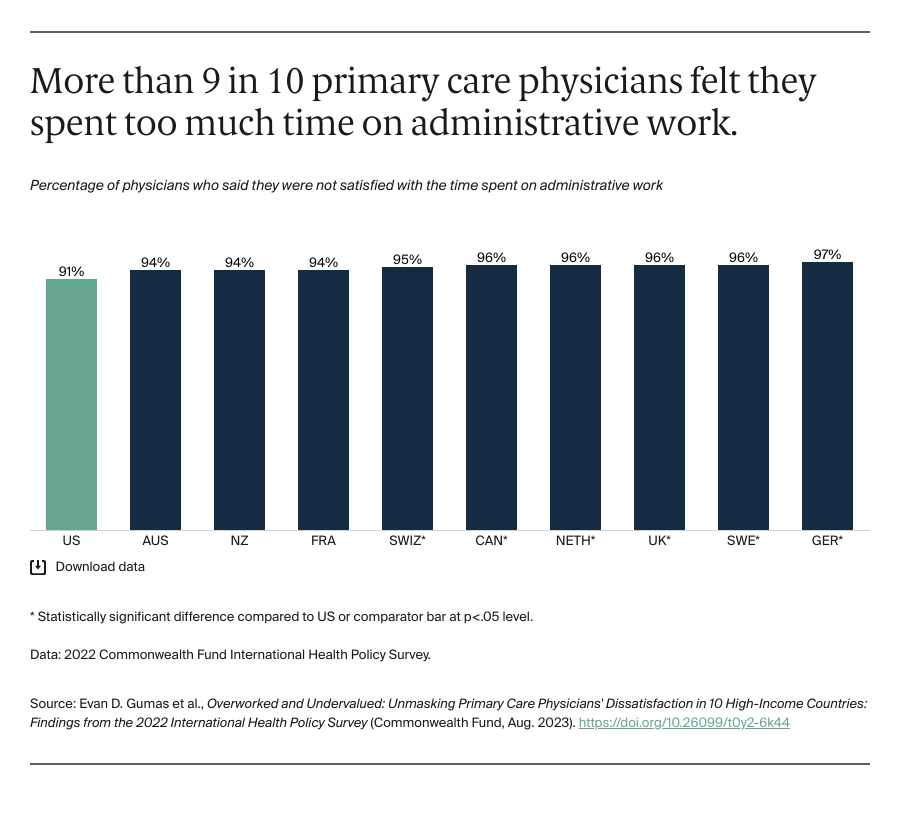
Consistent with prior research, results from our survey suggest primary care physicians have limited time to meet with patients and complete administrative tasks. This means they are not able to provide some patient services or deliver them in a way that is gratifying and according to care guidelines — all of which are tied to burnout and poorer patient outcomes.8 Studies have found that some physicians spend as much, if not more, time viewing the electronic health record of a patient as they do actually seeing the patient. While the information contained in electronic health records can facilitate more efficient care, its associated tasks can be cumbersome, at times undermining effective communication and connection in care settings.
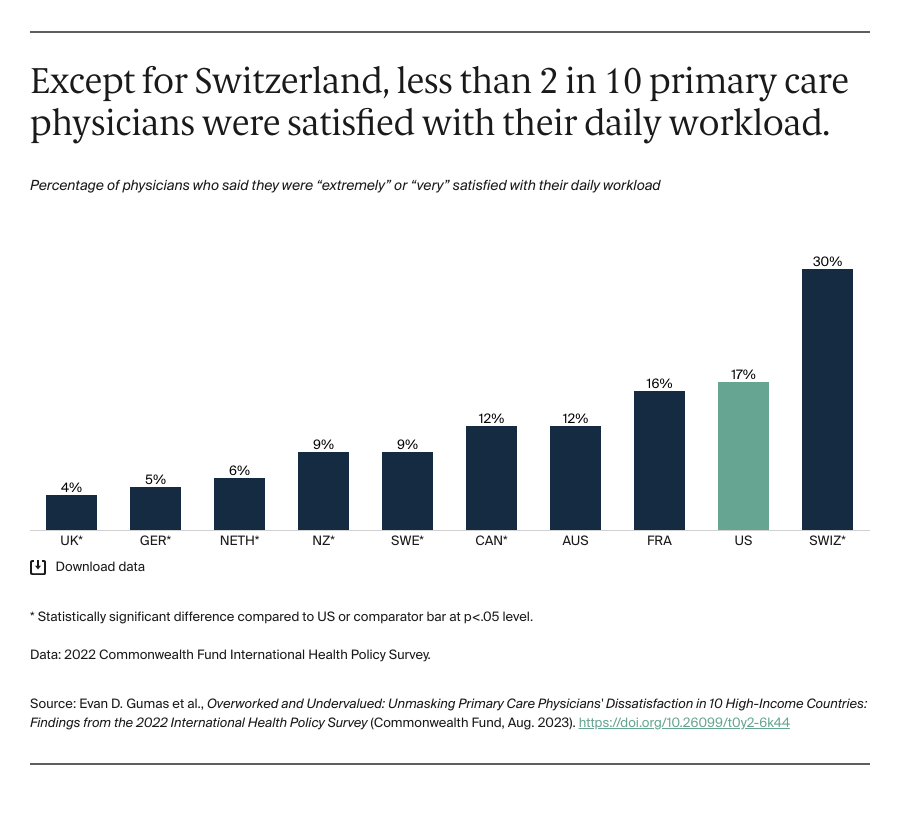
Reducing primary care physician workloads — something more than 80 percent of physicians in nearly every country reported struggling with — could increase satisfaction and lower high rates of stress and burnout. A 10 percent decrease in a physician’s workload in the United States has been shown to lower the odds of burnout by one-third.9 Strategies to streamline administrative work and reduce workload — as well as enhance care delivery — include redesigning health care information processing technology with the input of physicians. This could reduce time spent on maintaining electronic health records and other electronic administrative tasks.10
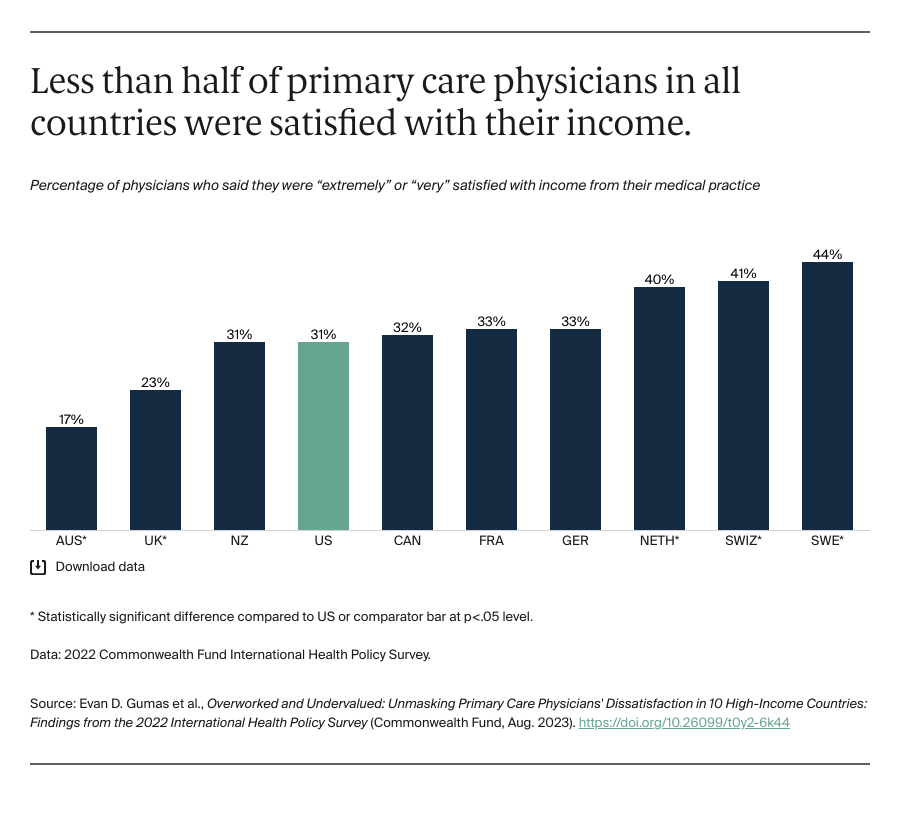
Restructuring reimbursement is another critical tool for improving primary care. Moving toward a value-based payment model, for example, can improve physician workloads by minimizing the need for administrative and billing work after the provision of services.11 By tying physician payment to health outcomes, value-based care also disincentivizes seeing a high volume of patients in favor of a comprehensive approach to patient care.12 Value-based reimbursements also could encourage more physicians to join the primary care workforce and foster an environment that supports career longevity.13
There is an undeniable crisis in primary care around the globe, and the U.S. is no exception. We cannot expect to receive the highest-quality care from physicians who are burned out, demoralized, and dissatisfied with core aspects of their work lives. By understanding how primary care physicians are feeling, particularly since the onset of COVID-19, we can gain insight into what they need in order to deliver high-quality patient care.