America has reached the one-year point in a complex, challenging undertaking with no real parallel in modern social welfare policy. On April 1, 2023, state governments, operating under broad Congressional and federal regulatory direction, began winding down continuous Medicaid enrollment, which had been adopted three years earlier at the beginning of the COVID-19 pandemic. Congress had elected this change to ensure Medicaid coverage would not be interrupted during the public health emergency but terminated it after it ended. Now that we’ve reached the one-year milestone in the unwinding process, it is valuable to reflect on its impact and assess whether it is time to stabilize Medicaid enrollment. Doing so would avert the frequent coverage interruptions that can seriously disrupt health care access.
Unwinding has had an enormous impact. Over three years, enrollment surged by more than 20 million people; by the start of unwinding, total enrollment was 94 million. States have completed about two-thirds of all scheduled renewals, but months of work remain. Among all beneficiaries completing the renewal process, slightly less than 70 percent (42.3 million people) have been successfully renewed while more than 19.6 million (slightly more than 30%) have lost coverage. Coverage losses appear driven by an apparent widespread failure in some states in the “ex parte” (i.e., streamlined, automated) Medicaid renewal process adopted under the Affordable Care Act (ACA), including a failure in the computer software program that is essential to making the process work.
The number of people who have lost coverage varies enormously across states; more than half of the people who went through the renewal process in Texas have lost coverage, compared to fewer than 22 percent in Illinois. Certain groups have been hit especially hard. For example, despite Medicaid’s relatively generous financial eligibility levels for children, more than 4 million children have lost coverage.
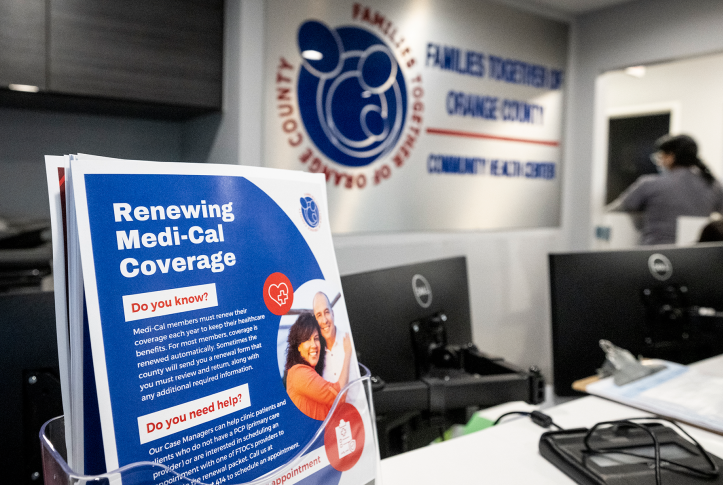
Furthermore, because Medicaid plays such an important role in supporting health care safety net providers like community health centers and women’s health clinics, the unwinding is having a significant financial and operational impact on clinics that care for people in medically underserved communities.
The following are key questions we will aim to answer as the unwinding process continues.
- How many of those people losing coverage remained eligible and in need of coverage? How many secured jobs with affordable workplace coverage or qualified for low-cost marketplace coverage? Advocates for low-income people have initiated legal challenges to the state unwinding process, suggesting that many people losing coverage remain eligible and in need of assistance.
- How many of those losing coverage ultimately made their way back into Medicaid? How long were they uninsured? Was their care affected in the interim?
- Why did renewal work reasonably well in some states and not others? Why did some states manage to achieve a high rate of automated renewals while other states failed and reverted to the old, flawed paperwork system?
- What happens to key groups that are not covered by the automated renewal process, such as children with special health care needs and adults with disabilities?
- Why did some states but not others take advantage of the special flexibilities afforded by Medicaid agencies during unwinding to ease the process for both workers and beneficiaries?
- Did some states’ decisions to proceed at higher speed — far faster than the unwinding process required — cause a higher rate of erroneous disenrollment?
- Did longstanding federal safeguards against unlawful and erroneous Medicaid terminations work? There has been troubling evidence in some states that showed a failure to review beneficiaries carefully and individually (e.g., reviewing children separately from their parents) to assess whether eligibility might continue?
- How did states’ underlying Medicaid eligibility choices — especially their decisions not to extend Medicaid eligibility under the ACA to all low-income working-age adults — affect older children and mothers who exhausted their postpartum eligibility period but had incomes that exceeded states’ financial eligibility limit for parents (e.g., as low as 16% of the federal poverty level in Texas)?
- Have states succeeded in coordinating the Medicaid renewal process with the insurance marketplace to ensure smooth transitions?
Above all, the unwinding underscores the urgency of addressing Medicaid’s most basic shortcoming — the absence of annual eligibility periods that can stabilize enrollment. Although the ACA streamlined renewals, this is no substitute for annual eligibility periods. Streamlined renewal procedures cannot overcome unstable underlying eligibility rules that can cost people coverage at any time for slight changes in income or family circumstances. If — prior to the pandemic — Medicaid enrollment had been on an annual basis, we would not have the problem of frequent eligibility churn and the task of resuming normal Medicaid operations would have been greatly simplified. Guaranteeing stable, uninterrupted insurance coverage for the poorest Americans was crucial to protecting access to care during the public health emergency. The effort required to patch over this basic shortcoming and restart a flawed process shows the urgency of a solution.
Medicaid is the nation’s largest public insurer and most important public health first responder. It was designed to serve as a vital health care safety net for all eligible people when care is needed, and it continues to play this vital role for millions. It is now time for policy reforms to address enrollment stabilization, which would recognize that Medicaid is a critical point-of-need safety net but also an ongoing insurer for millions.