In our previous discussion, we explored how various countries successfully implement diverse health care models to achieve universal coverage. From Switzerland’s private insurance to Singapore’s health savings accounts and other more socialized systems, each offers unique lessons on balancing public and private involvement in health care coverage. Now, let’s pivot our focus to the United States.
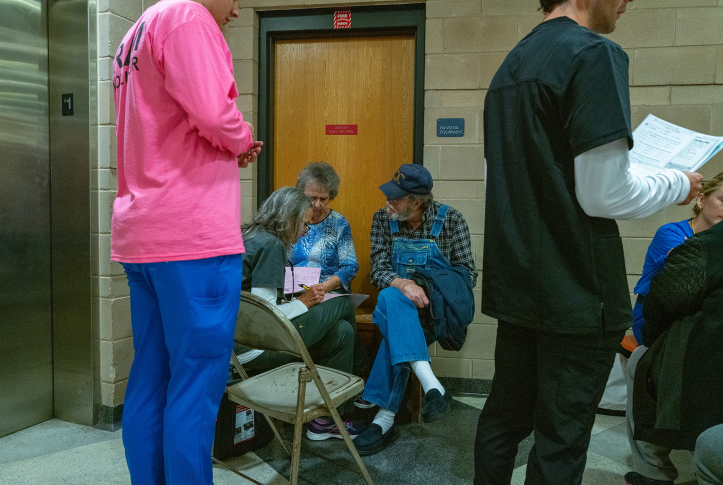
The U.S. health care system is a complex patchwork that seems to combine the worst of all worlds. Employer-based insurance limits choice by tying coverage to employment. Medicare is akin to a single-payer system but comes with its own challenges, including high out-of-pocket costs for specific services and medications. The VA system, which provides care for military veterans, is the closest the United States comes to a thoroughly socialized system, like England’s National Health Service (NHS). However, it has significant challenges, including long wait times and questions about quality. The Medicaid model provides a safety net for vulnerable populations. Still, eligibility and the range of services covered vary significantly from state to state, resulting in a patchwork that can be confusing and inadequate.
This complexity isn’t just confusing; it’s inefficient. It often fails to meet our two main goals: access and financial protection. The fragmented nature of the American system creates gaps in coverage, inconsistencies in treatment, and inefficiencies that drive up costs for everyone.
While we’re engrossed in debates about coverage systems, though, we’re overlooking another crucial aspect: the delivery of health care services. How do we ensure that the care we’re paying for is not just accessible but also effective, efficient, patient-centered, and equitable?
Public vs. Private: A False Dichotomy
The notion that the private sector is inherently superior to the public sector is flawed. While some believe the private sector emphasizes innovation and customer service, it often comes at a steeper price. It values choice and individual preferences but can lead to disparities. Those with fewer means are often unable to attain needed care, and evidence shows that race, ethnicity, and gender can affect the access and quality of care that patients experience.
Conversely, the public sector can often be more outcome-driven and cost-effective, but it might not always offer the latest innovations or personalized experiences. It’s often designed to provide a baseline of quality care for all but might not always have the resources or incentives to push boundaries or provide amenities.
In the U.S., there’s a significant tilt toward private delivery systems, which can lead to higher costs while not necessarily delivering better outcomes. To achieve a more efficient and equitable system, the U.S. should consider striking a balance, like other developed countries have done.
Striking a Balance
The United Kingdom, France, Australia, New Zealand, and Singapore predominantly rely on public delivery systems, ensuring that most of their populations have access to quality care without exorbitant costs. Public delivery systems can become overloaded, though, with long waiting lists. So, these countries maintain a private “release valve” for people seeking quicker access, specialized treatments, or more luxurious accommodations. If people are willing to pay more and can get care elsewhere, they leave fewer patients waiting in line in the public system.
In the U.K., the NHS offers a robust public system that delivers good care at a much lower cost, but patients can also use the private system for expedited access to specialists or nicer hospital accommodations. However, when too many patients choose not to use the private system, the public system can become overloaded. In the U.K., this has resulted in overwhelmed emergency rooms at times.
In France, an outpatient physician visit costs €25, most of which is covered by insurance. Balance billing is available for the few physicians who charge more, but that amount is made clear to patients upfront. The inpatient sector leans heavily public, ensuring access to essential care without financial strain. This dual approach allows France to maintain high standards of care while also offering patients choice. Australia and New Zealand have similar models, with a primarily private outpatient sector and a primarily public inpatient sector.
Expanding the Definition of Health Care
In the U.S., health care discussions and spending are predominantly centered on acute care and physician services. Even when we talk about “preventive care,” it’s often limited to the confines of a doctor’s office. This perspective fails to acknowledge the many factors that play a role in health, like housing, education, transportation, food security, safety, and access to social services.
Other nations have adopted a more comprehensive view. Singapore, for instance, has invested significantly in public housing, recognizing the link between stable, quality housing and overall health. New Zealand has been proactive in addressing the unique health needs of the Māori community to ensure culturally attuned health services. France has expanded its definition of preventive care and now incorporates home visits for new mothers and a broad spectrum of sexual health services.
The Cost-Effectiveness of Prevention
In the United States, we assume that public health initiatives should both improve outcomes and save money. Other countries realize that prevention might not always be cost-saving in the immediate term but it is often massively cost-effective in the long run. This includes vaccination programs, antismoking campaigns, and interventions like bolstering sanitation or promoting clean water access. In addition, programs targeting the early stages of life, such as prenatal care and early childhood education, have produced significant long-term health benefits. The Nurse–Family Partnership program in the U.S. has demonstrated that nurse home visits for first-time mothers can lead to improved health and development for mothers and children.
Time for a New Conversation
The American health care debate needs a reboot. We must move beyond the arguments that have dominated the discourse for decades and instead look to the successful approaches of other countries. We can achieve universal coverage, invest in public delivery systems, and broaden our understanding of health care to include preventive services, public health initiatives, and the social drivers of health. These will make more of a difference than a simple change to a single-payer system.
By learning from other countries, we can build a better, more inclusive health care system that accomplishes enough for all while allowing some the choice to pay for more. But to do that, we need to have a better conversation — one that is informed, nuanced, and open to new ideas.