The Biden administration recently finalized its long-awaited revision to the regulations governing section 1557 of the Affordable Care Act (ACA). These regulations represent a major advance toward the ACA’s goal of nondiscrimination in health coverage and care, but progress is delayed by federal courts. Just before the new regulations’ effective date, three federal courts put various provisions on hold, with one order applying nationwide. This post describes provisions of the new regulations and explains the recent court orders delaying implementation.
Section 1557’s Prohibition Against Discrimination in Health Coverage and Care
Section 1557 prohibits health programs or activities that receive federal financial assistance from discriminating on race, color, national origin, sex, age, or disability. Examples of entities covered by section 1557 include health care providers, health insurers, and state Medicaid agencies. Section 1557 also bans discrimination in health programs or activities administered by federal agencies and the marketplaces. By including section 1557 in the ACA, Congress recognized that discrimination could contribute to poor health outcomes and worsen disparities, and that remedying discrimination helps further the ACA’s goal of expanding access to health coverage and care.
This lesser-known provision of the ACA is noteworthy because it is the first federal law banning discrimination based on sex in health care. Prior to the enactment of the ACA in 2010, it was entirely legal to treat patients or health insurance enrollees differently based on sex, by charging higher premiums, for instance. Section 1557 also recognizes claims of intersectional discrimination. By bringing together preexisting federal civil rights laws that ban discrimination in health care and adding sex as a protected basis, section 1557 recognizes that individuals can be uniquely harmed by discrimination that touches on multiple identities or traits protected by federal law, such as a pregnant person with a disability or a transgender person of color.
Key Provisions of the New Regulations
The Biden provisions are the third version of the section 1557 regulations, preceded by the original Obama regulations in 2016 and the Trump regulations in 2020. In several respects, the new regulations reverse provisions of the 2020 regulations and reinstate provisions originally adopted by the 2016 regulations. These include:
- Restoring gender identity as part of the sex discrimination definition. The new regulations again recognize gender identity as part of section 1557’s prohibition against sex discrimination. They also reinstate provisions that prohibit covered entities from denying or limiting individuals’ access to health care services based on gender identity. The future of these provisions is uncertain due to lawsuits challenging the regulations.
- Health insurance. Health insurers again are explicitly prohibited from denying or limiting coverage or claims, canceling or refusing to renew coverage, or imposing additional cost sharing based on race, color, national origin, sex, age, or disability. The new regulations also restore prohibitions on discriminatory plan marketing and benefit design. For example, insurers cannot assign all drugs to treat a certain medical condition to a health plan’s highest cost-sharing tier. Furthermore, section 1557 again applies to all operations of a health insurance issuer that receives federal funding. By contrast, the 2020 regulations narrowed section 1557 to apply only to specific health plans that directly received federal funding.
- Meaningful access for individuals with limited English proficiency. The regulations reinstate a focus on language access for individuals with limited English proficiency (as opposed to a general obligation regarding language access) as well as covered entities’ obligation to notify individuals about the availability of free language assistance services, provide auxiliary aids and services for people with disabilities, and provide taglines (i.e., short statements indicating the availability of free language assistance services) in the 15 most spoken languages.
- Association-based discrimination. The new regulations reinstate the prohibition against discrimination based on an individual’s association with another person, based on that person’s race, color, national origin, sex, age, or disability. For example, a doctor cannot refuse to see a white patient because that patient has a biracial child.
- Notices and procedures. Covered entities again must provide nondiscrimination notices to individuals. Additionally, the new regulations restore the obligation of entities with 15 or more employees to implement written grievance procedures and designate an employee to coordinate section 1557 compliance.
Notably, the new regulations also include some provisions that are more expansive than the 2016 regulations, such as:
- Broader sex discrimination definition. The new regulations expand the definition of sex discrimination to include sexual orientation.
- Application of religious freedom and conscience laws. The new regulations acknowledge that covered entities are protected by other federal laws that allow health care refusal based on a provider’s religious or conscientious objections. The new rules adopt an optional process for covered entities with religious or conscientious objections to obtain assurance from the U.S. Department of Health and Human Services (HHS) that they are exempt from compliance with section 1557 for specific contexts, procedures, or services. Unlike the 2020 regulations, the new regulations do not incorporate a blanket religious freedom exemption.
- Telehealth and patient care support tools. Covered entities cannot discriminate when delivering services through telehealth or using patient care support tools to assess health status, recommend care, or conduct utilization reviews.
- Broader federal funds definition. The new rule recognizes receiving Medicare Part B funding as subjecting an entity to section 1557, similar to other federal funds, like Medicare Part A, Medicaid, and marketplace subsidies.
- Training. Covered entities must train employees on civil rights policies and procedures.
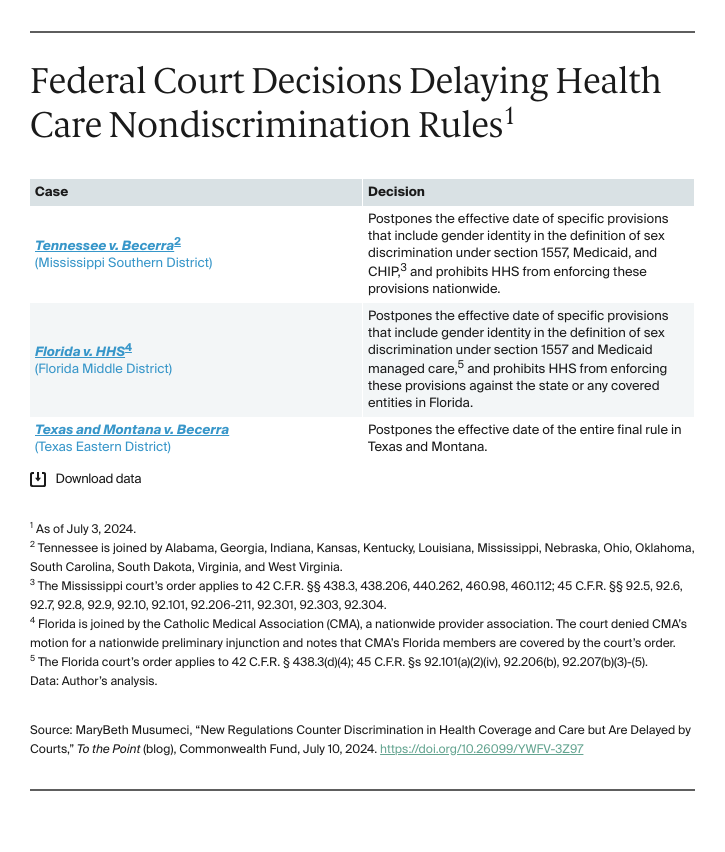
Federal Court Decisions Delaying the New Regulations
The new regulations were scheduled to take effect on July 5, 2024. However, on July 3, 2024, a Mississippi federal court postponed the effective date of certain provisions that include gender identity in the definition of sex discrimination and prohibited HHS from enforcing those provisions nationwide. That same day, another federal court prohibited HHS from enforcing a subset of provisions that include gender identity in the definition of sex discrimination in Florida, while a third federal court postponed the effective date of the new rule in its entirety in Texas and Montana. HHS can appeal these decisions. However, as noted multiple times in all three decisions, HHS’s interpretation of section 1557 is no longer entitled to judicial deference, as a result of the Supreme Court’s recent ruling in Loper Bright v. Raimondo. At best, full implementation of the section 1557 regulations will be delayed by years of litigation; at worst, section 1557 will fall far short of its potential to remedy health disparities resulting from discrimination.