In 2022, more than 2.71 million hospitalized Medicare patients (21%) — both traditional Medicare and Medicare Advantage beneficiaries — received a referral for home health care. But research suggests many did not receive their needed care. Data from 2016 show that only 54 percent of hospitalized Medicare beneficiaries referred for home health care received it. Low fulfillment rates for home health referrals can lead to patients being readmitted to the hospital and sometimes death. In this blog post, we look at how many hospitalized Medicare patients received home health care, even when referred for it, and how those rates differ across beneficiaries’ gender, race, dual eligibility status, and geography.
Fewer Hospitalized Beneficiaries Referred to Home Health Receive Services
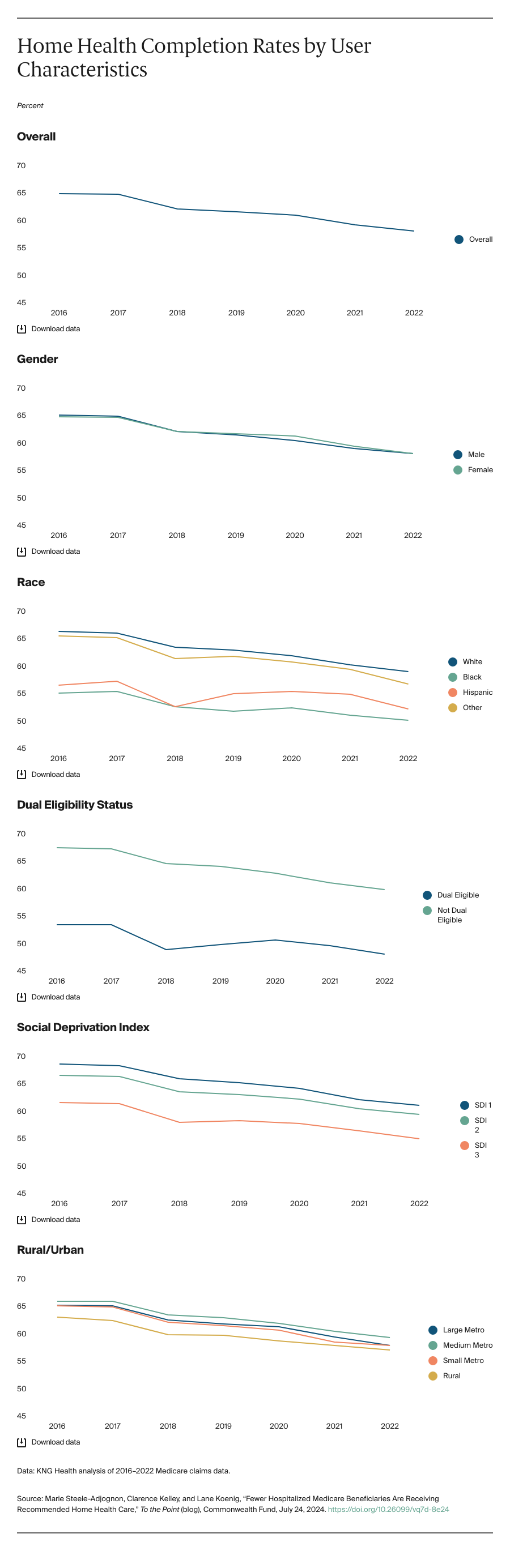
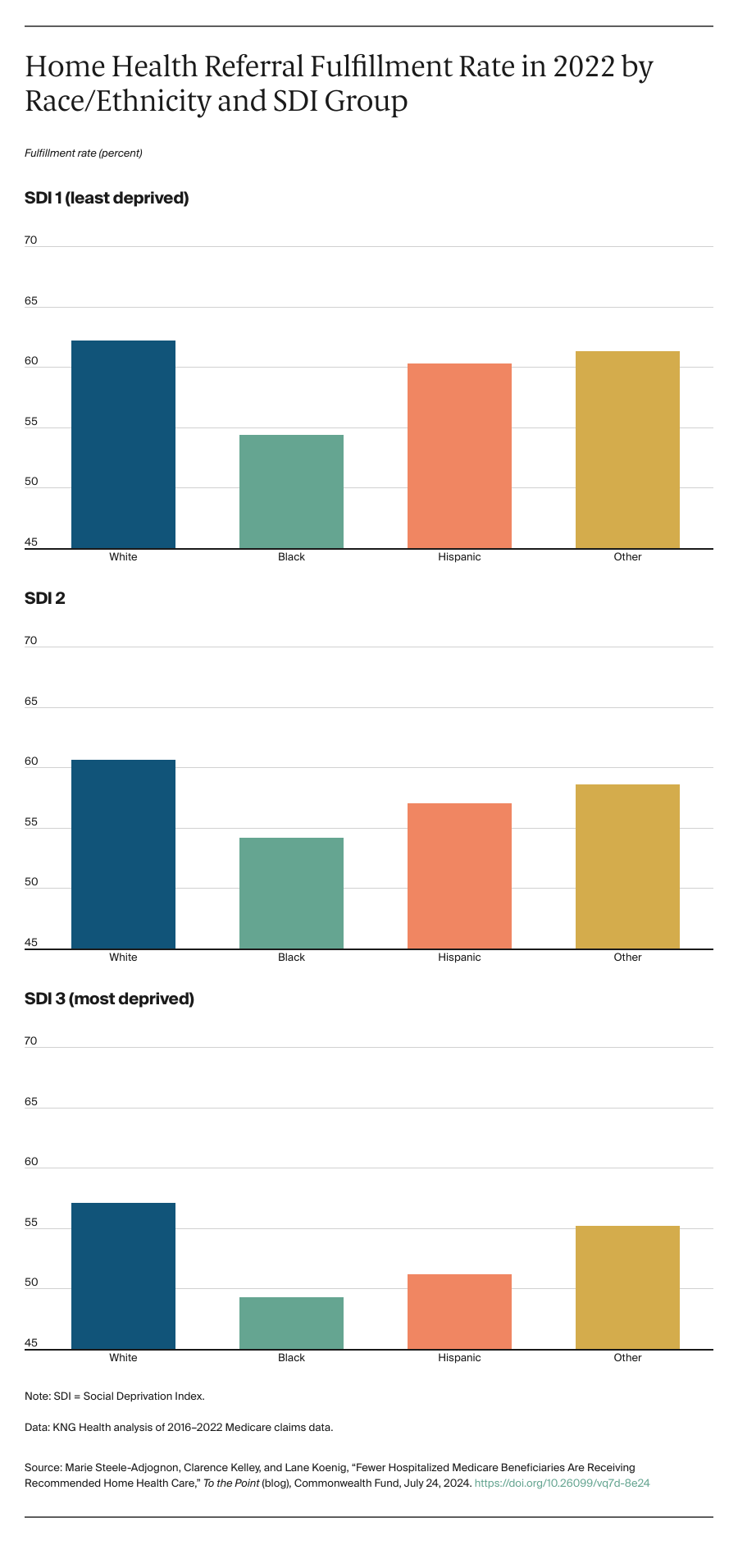
Overall home health referral fulfillment rates decreased from 66 percent to 59 percent between 2016 and 2022. This trend was observed before and during the COVID-19 public health emergency and occurred across all racial and ethnic groups. The overall decrease was largely driven by the significant decline (7.2 percentage points) in the rate for white beneficiaries. We observed racial and ethnic disparities in fulfillment rates over that period, although they narrowed slightly. Beneficiaries dually enrolled in Medicare and Medicaid had lower rates of home health referral fulfillment compared to those not dually enrolled. (All differences reported above were statistically significant at the 5 percent level.)