The Issue
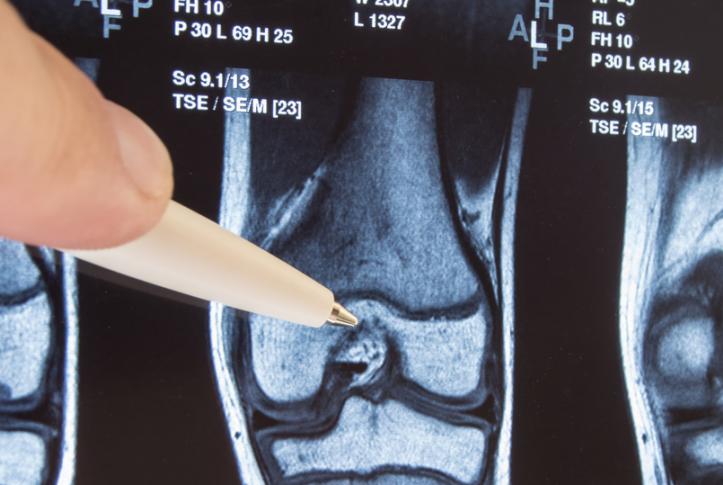
In 2013, the Centers for Medicare and Medicaid Services (CMS) introduced a voluntary program for hospitals called Bundled Payments for Care Improvement (BPCI). Under this alternative payment model, CMS makes a single, preset payment for an episode, or “bundle,” of care, which may include a hospitalization, postacute care, and other services. Evaluations of the program for lower extremity joint replacement surgery (e.g., a hip or knee replacement) have found that it reduced spending. But experts wonder if bundled payments could encourage hospitals to perform more surgeries than they would otherwise or to cherry-pick lower-risk patients. Commonwealth Fund–supported researchers explore these issues of volume and case mix in the Journal of the American Medical Association. The authors used Medicare claims data from before and after the launch of BPCI, comparing markets that did and did not participate in the program.
What the Study Found
3.8% increase in mean quarterly market volume in non-BPCI markets after the program was launched 4.4% increase in mean quarterly market volume in BPCI markets after the program was launched
- Participation in the BPCI program was not significantly associated with an overall change in the volume of surgeries performed.
- The mean quarterly market volume in non-BPCI markets increased 3.8 percent after the program was launched. For BPCI markets, the increase was 4.4 percent.
- The analysis found only one change in case mix: patients who had previously used skilled nursing facilities were slightly less likely to undergo a lower extremity joint replacement surgery at a hospital participating in BPCI.
The Big Picture
Results from this study alleviate concerns that hospitals’ participation in voluntary bundles may increase the overall number of joint replacement surgeries paid for by Medicare. In particular, the savings per episode observed in prior BPCI evaluations are not diminished or eliminated by an increase in procedure volume. The findings do raise concerns: if patients with prior use of skilled nursing facilities are less likely to undergo procedures at BPCI-participating hospitals, perhaps it is because hospitals avoid them based on perceived risk. On the other hand, the authors note, these decisions could have been based on clinically appropriate factors, like risk of complications.
The Bottom Line
Hospital participation in a bundled care program did not change overall volume, thereby alleviating the risk of eliminating savings related to the program. In addition, participation was generally not associated with changes in case mix.