Data Sources and Methods
Organisation for Economic Co-operation and Development
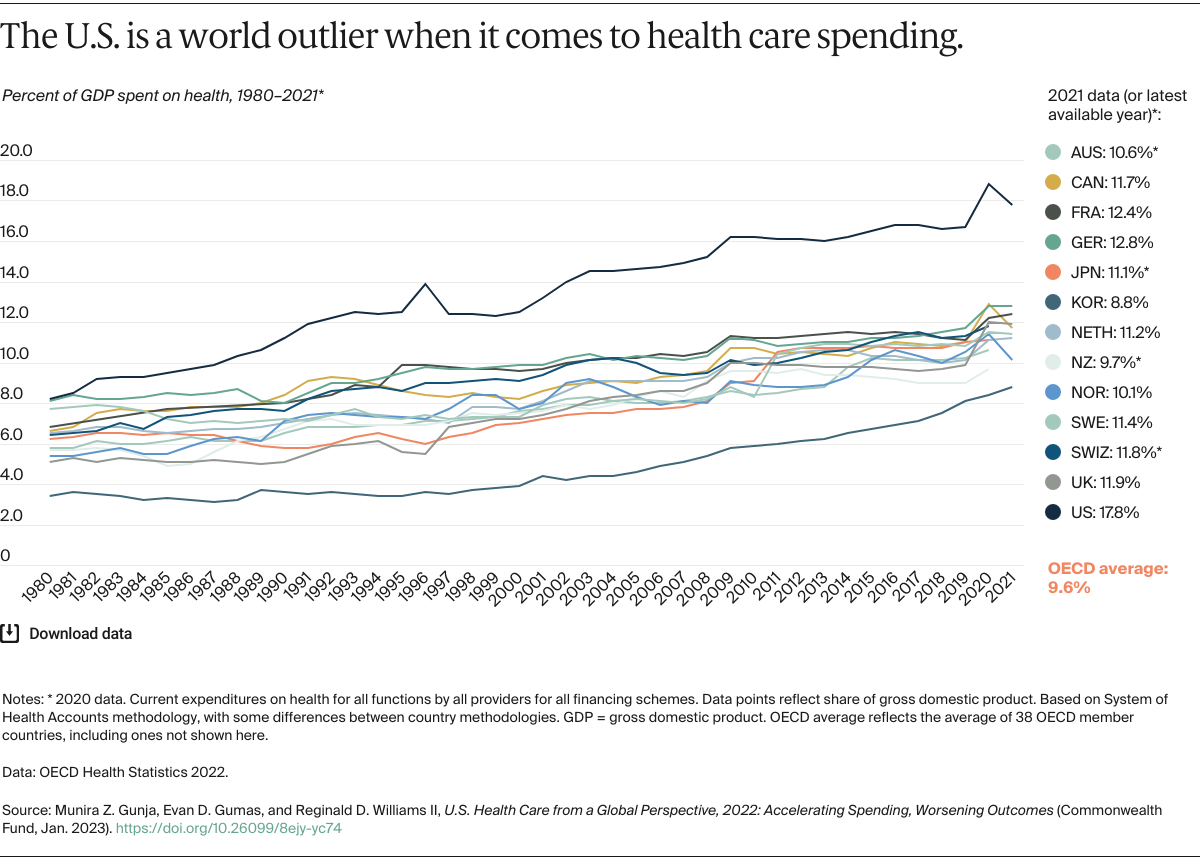
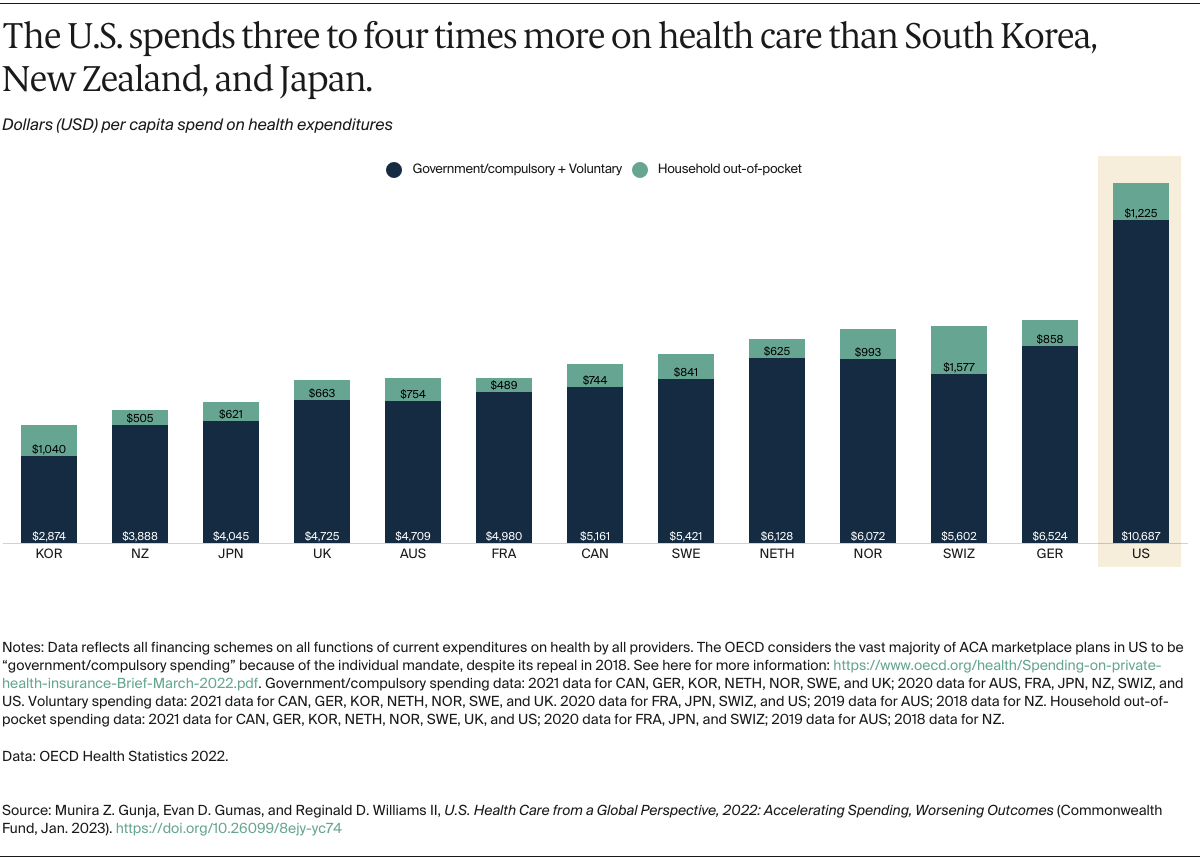
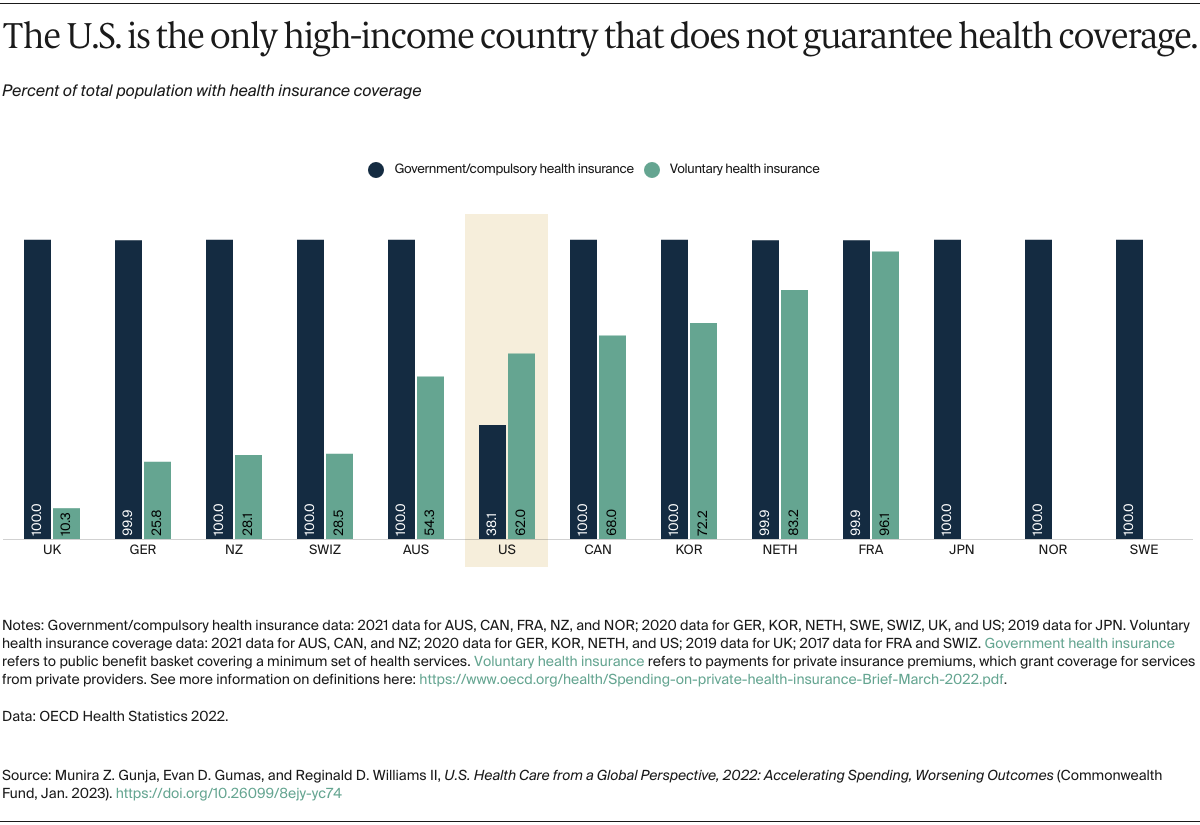
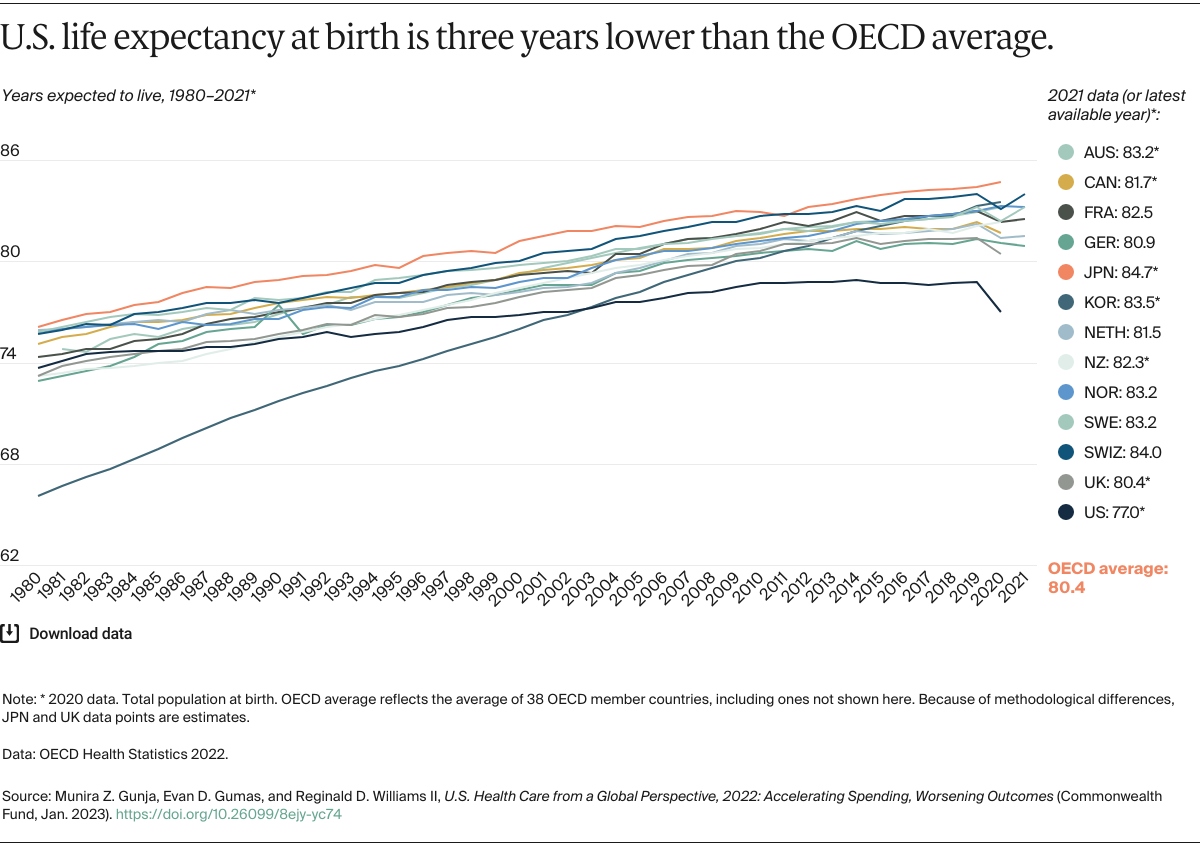
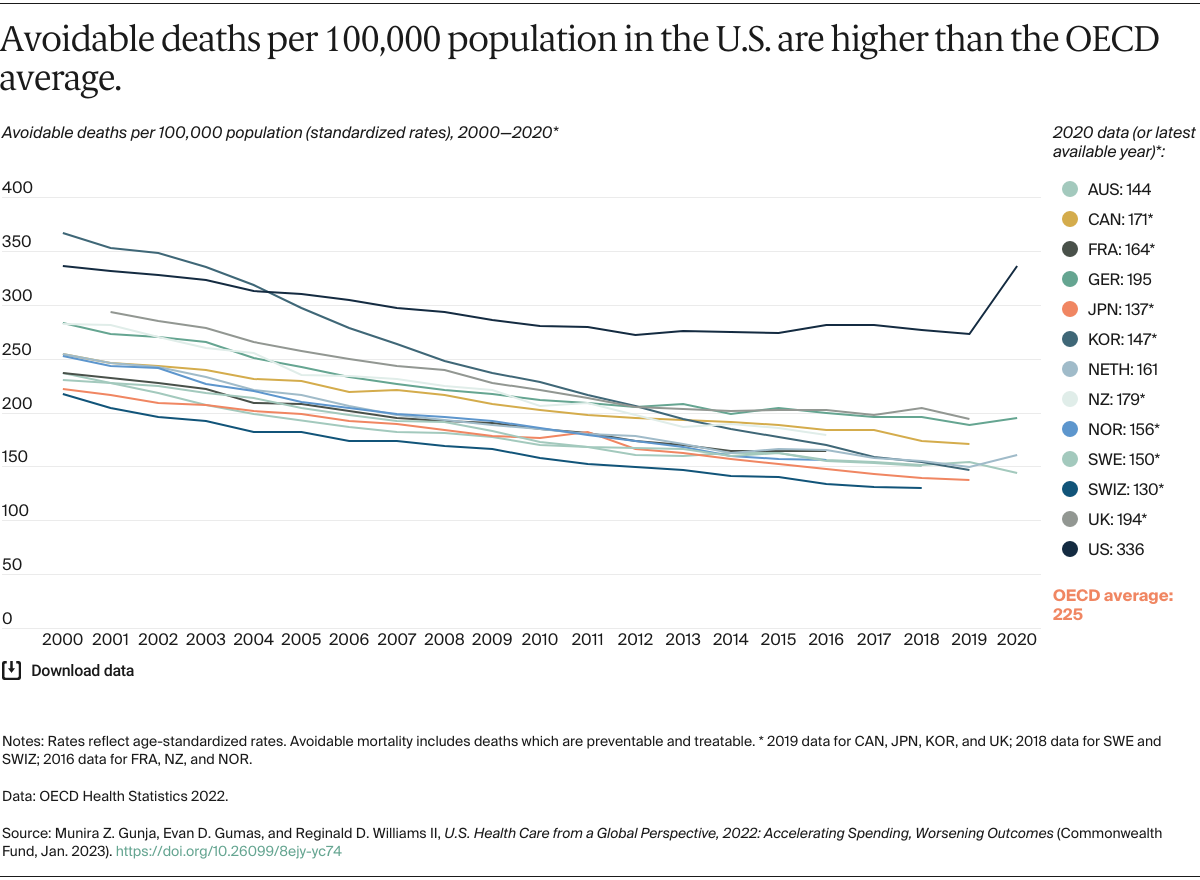
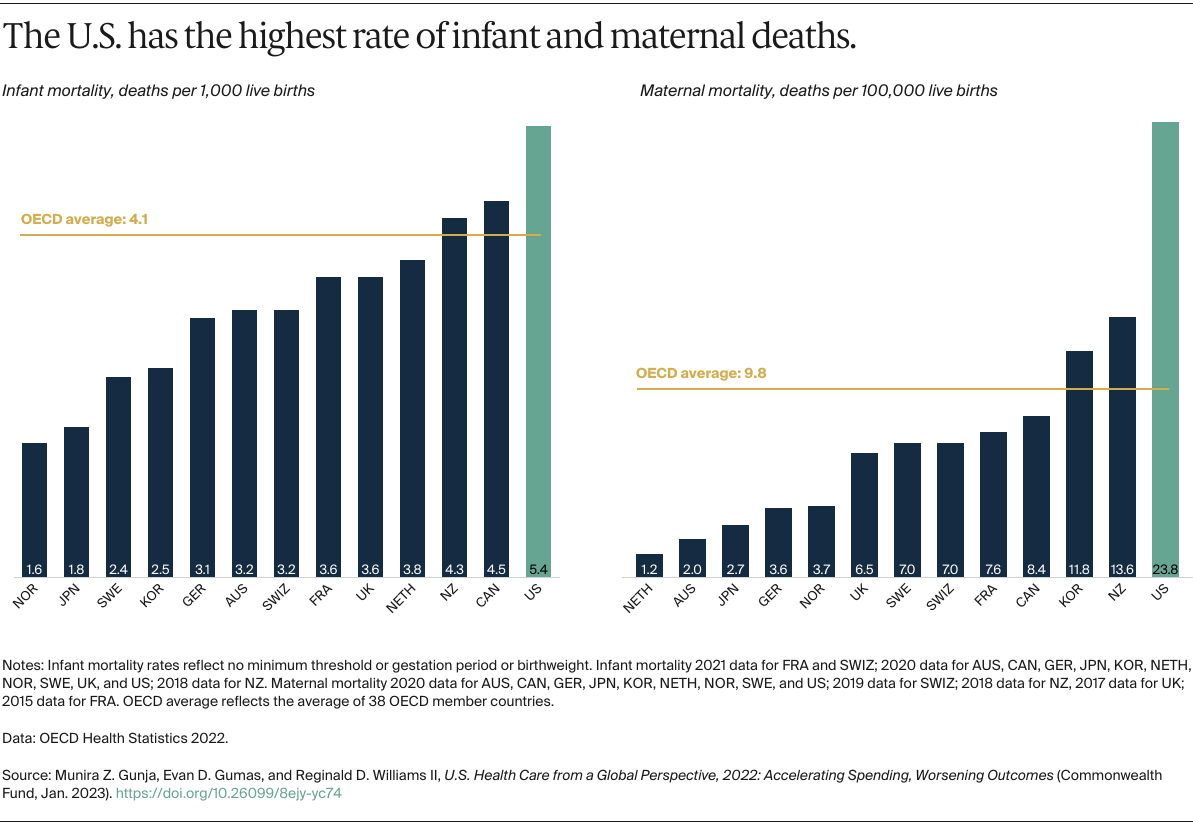
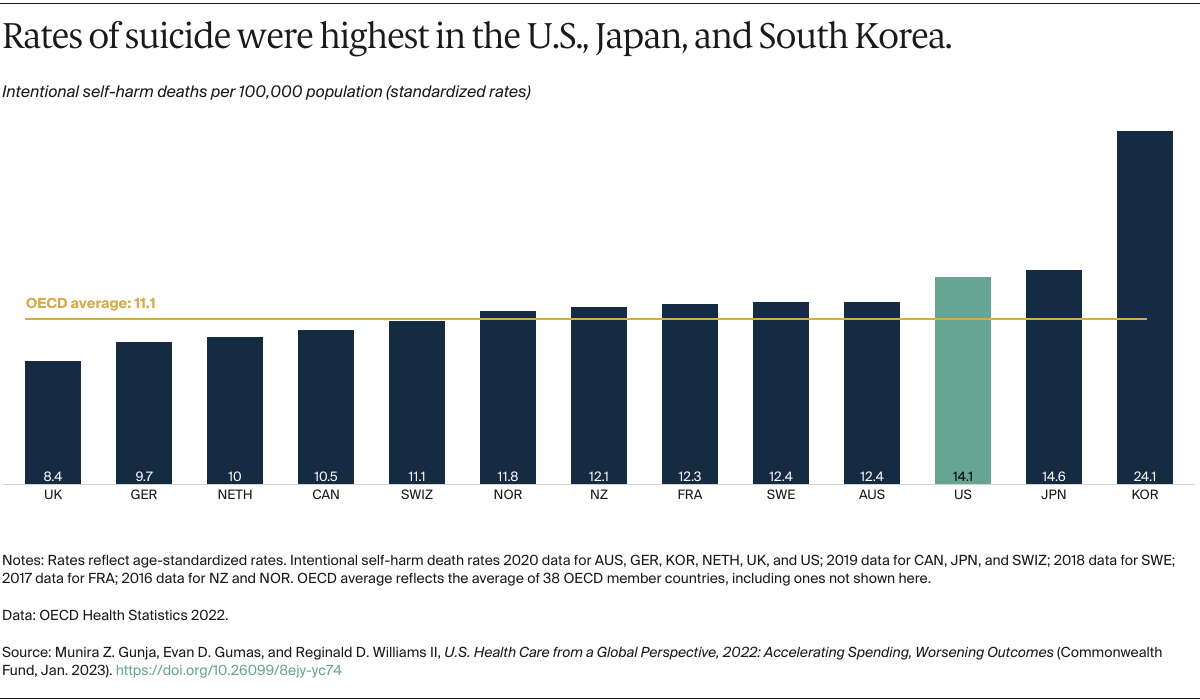
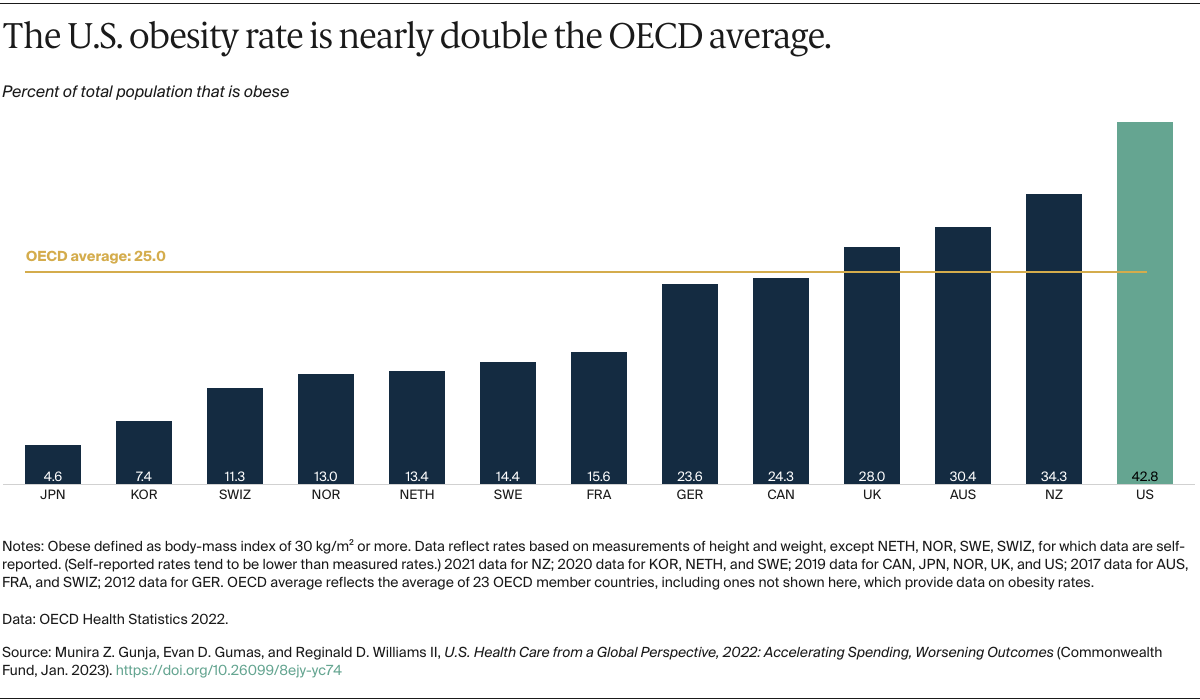
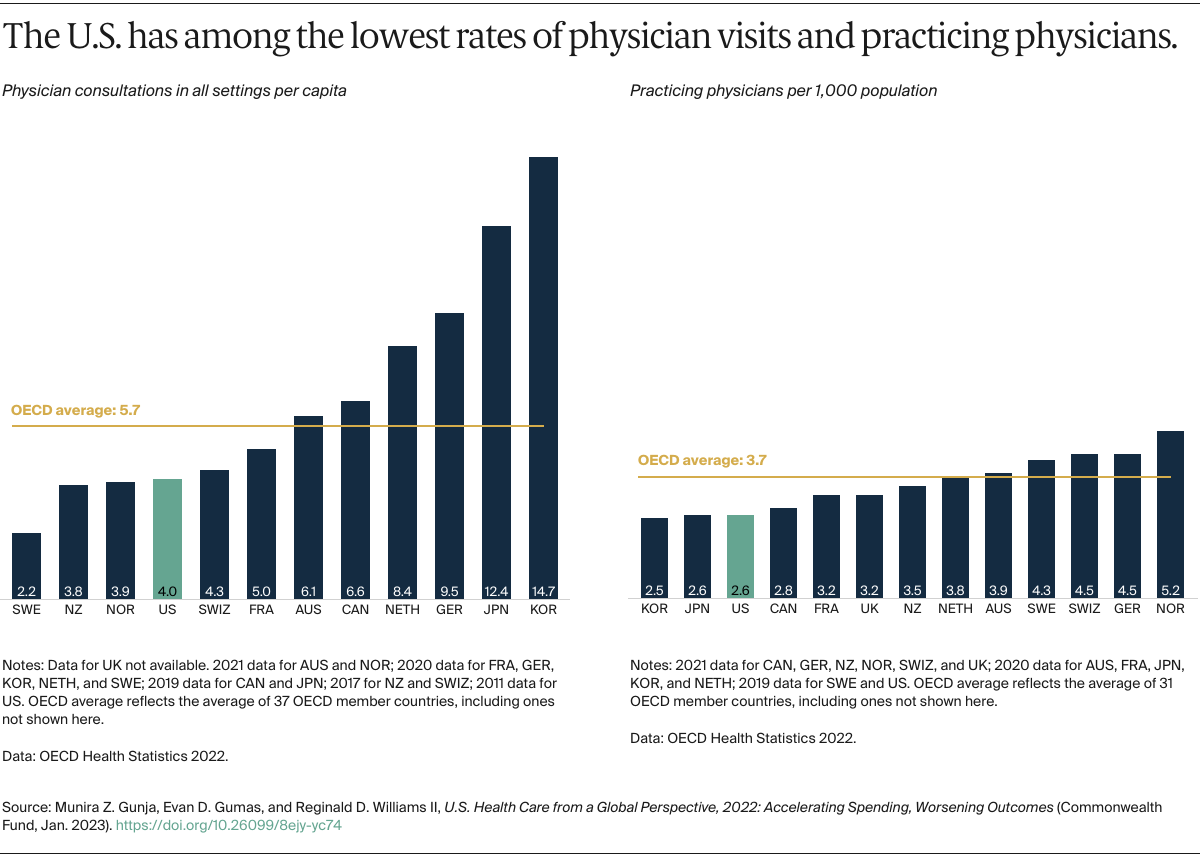
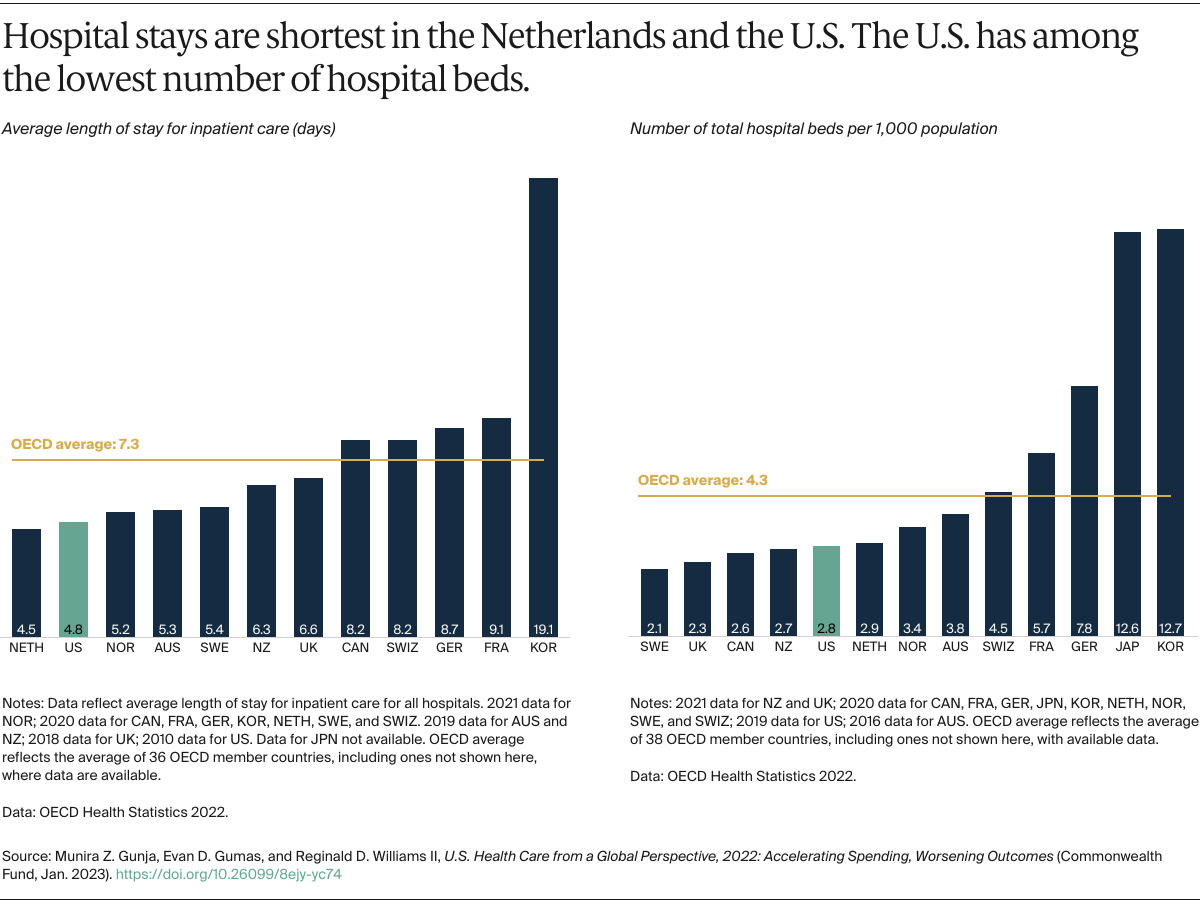
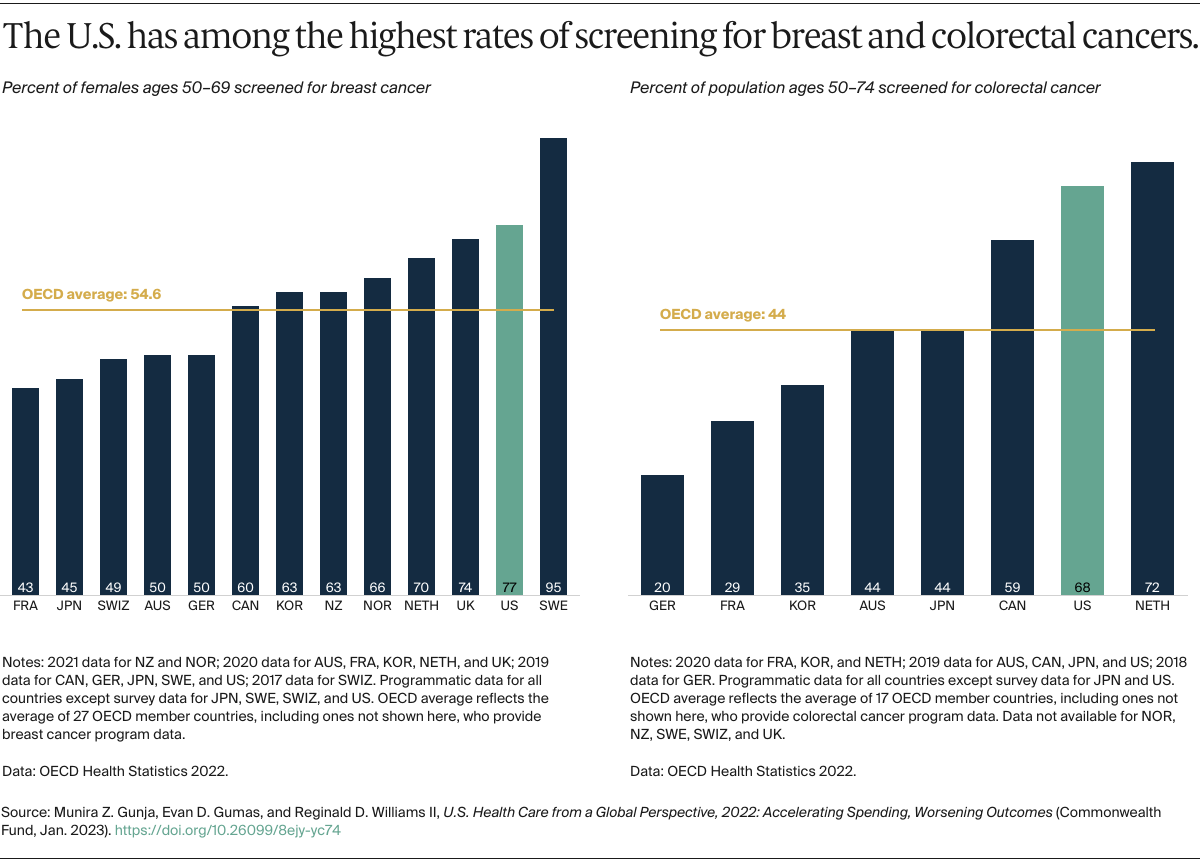
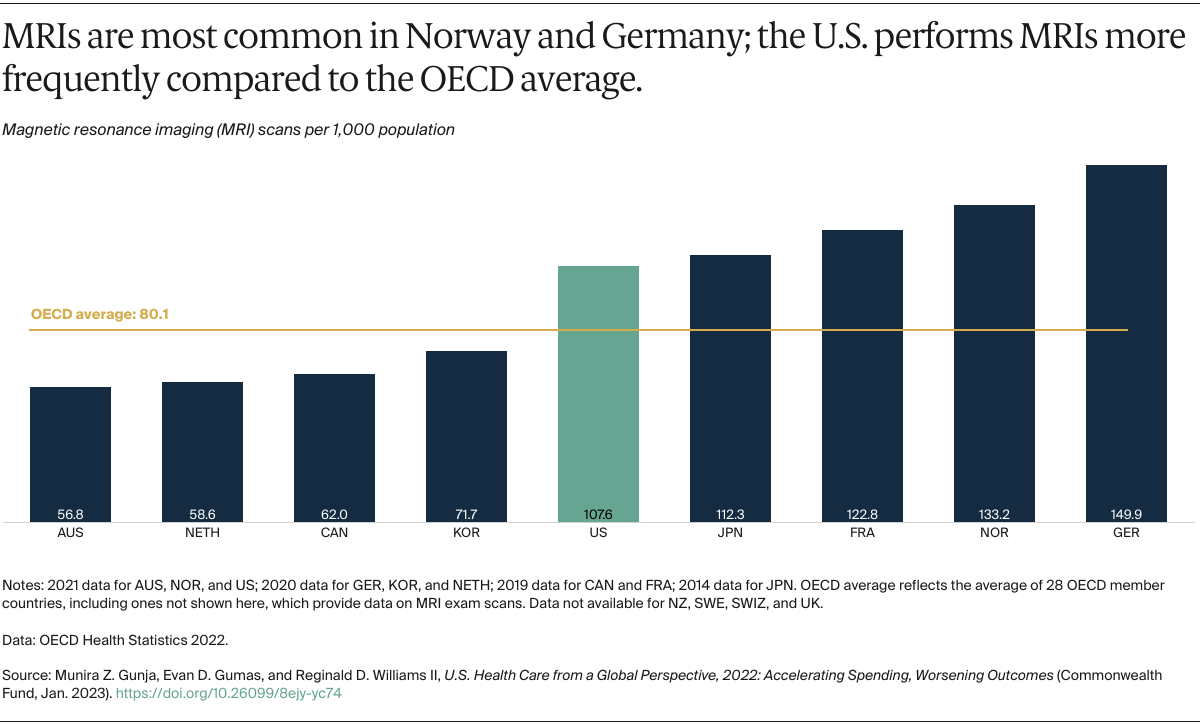
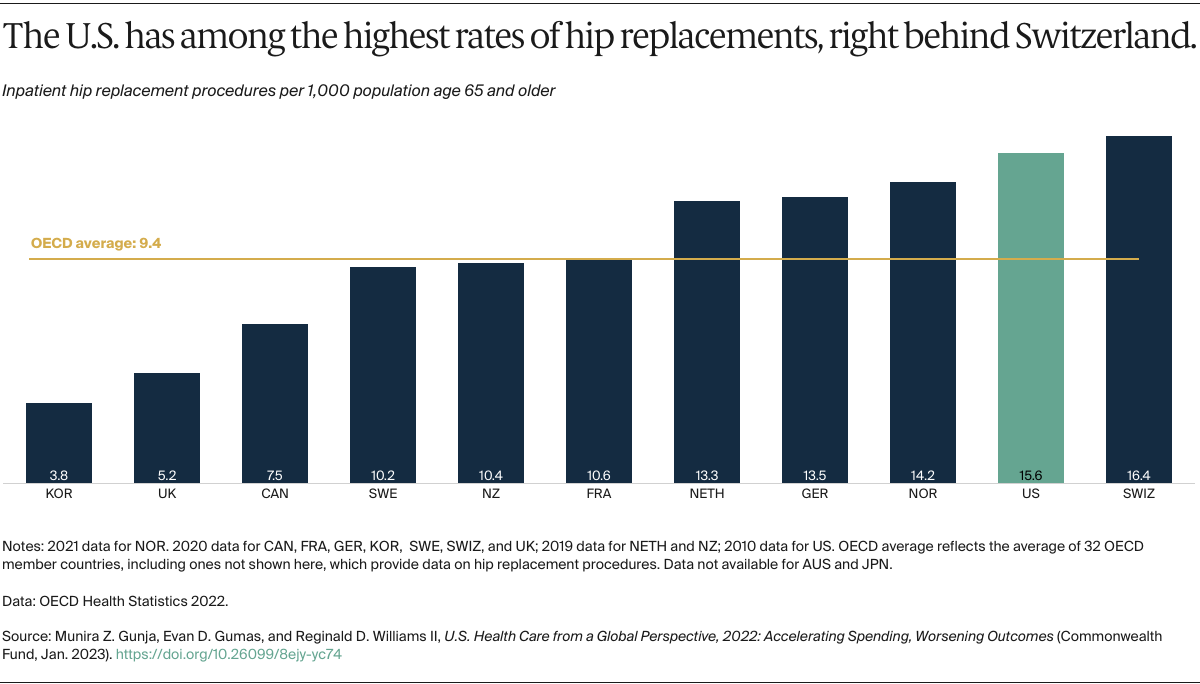
This analysis used data from the 2022 release of health statistics compiled by the Organisation for Economic Cooperation and Development (OECD), which tracks and reports on a wide range of health system measures across 38 high-income countries. Data were extracted in December 2022. While data collected by the OECD reflect the gold standard in international comparisons, one limitation is that data may mask differences in how countries collect their health data. Full details on how indicators were defined, as well as country-level differences in definitions, are available from the OECD.24
2020 Commonwealth Fund International Health Policy Survey
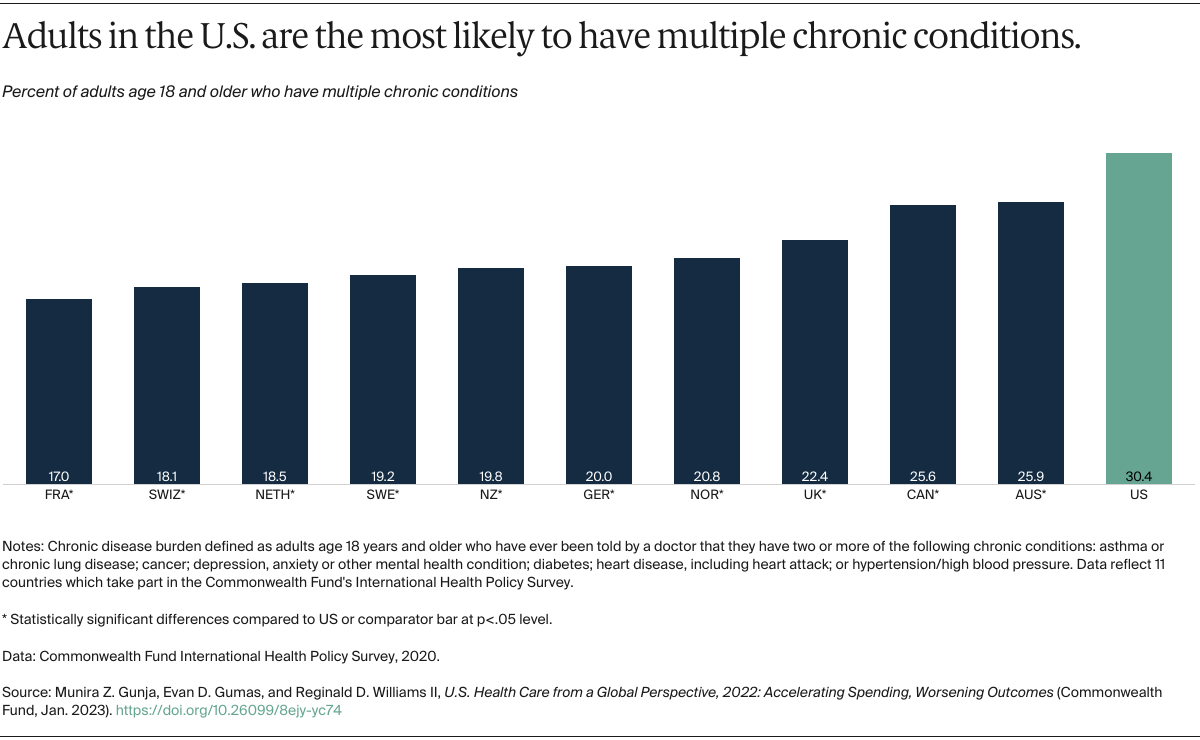
For the 2020 Commonwealth Fund International Health Policy Survey, data were collected from nationally representative samples of noninstitutionalized adults age 18 and older in Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Switzerland, Sweden, the United Kingdom, and the United States. Samples were generated using probability-based overlapping landline and mobile phone sampling designs in all but three countries. In Norway, Sweden, and Switzerland, respondents were randomly selected from listed or nationwide population registries. In the U.S., an address-based sampling frame was also incorporated to ensure a representative sample of respondents. Respondents completed surveys via landline and mobile phones, as well as online, in Sweden, Switzerland, and the U.S.
International partners cosponsored surveys, and some supported expanded samples to enable within-country analyses. Final country samples ranged from 607 to 4,530 participants. The survey research firm SSRS was contracted to conduct the survey with country contractors from February through May 2020. The field period across countries ranged from four to 15 weeks. Response rates varied from 14 percent to 49 percent. Data were weighted using country-specific demographic variables to account for differences in sample design and probability of selection.
Our World in Data
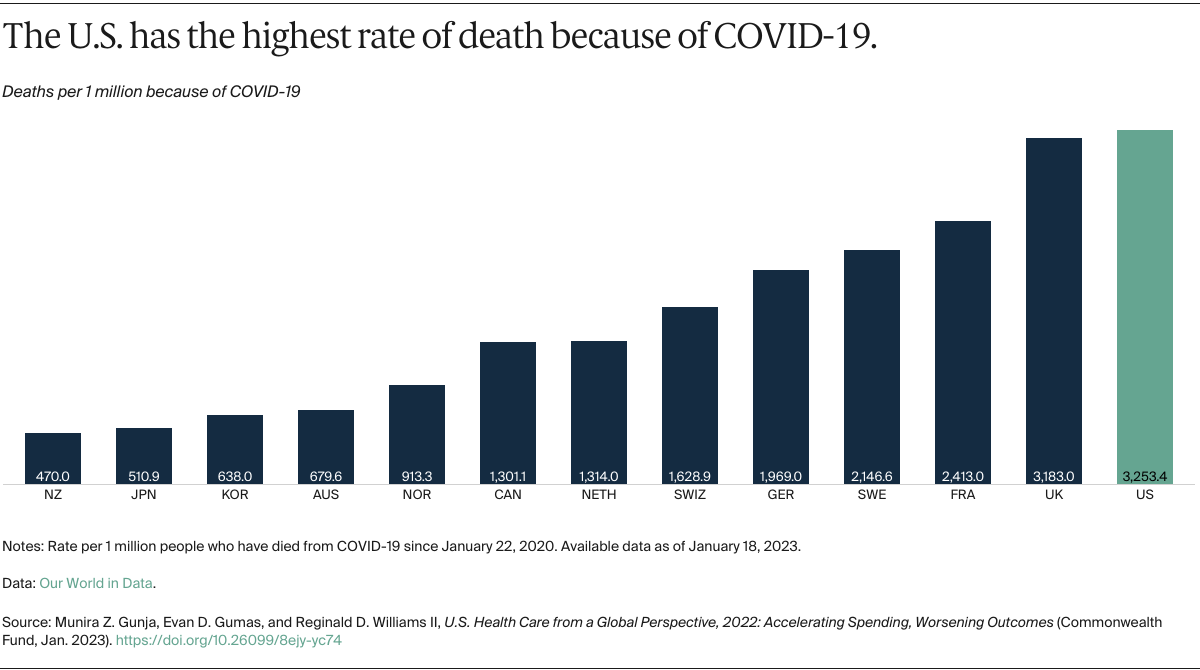
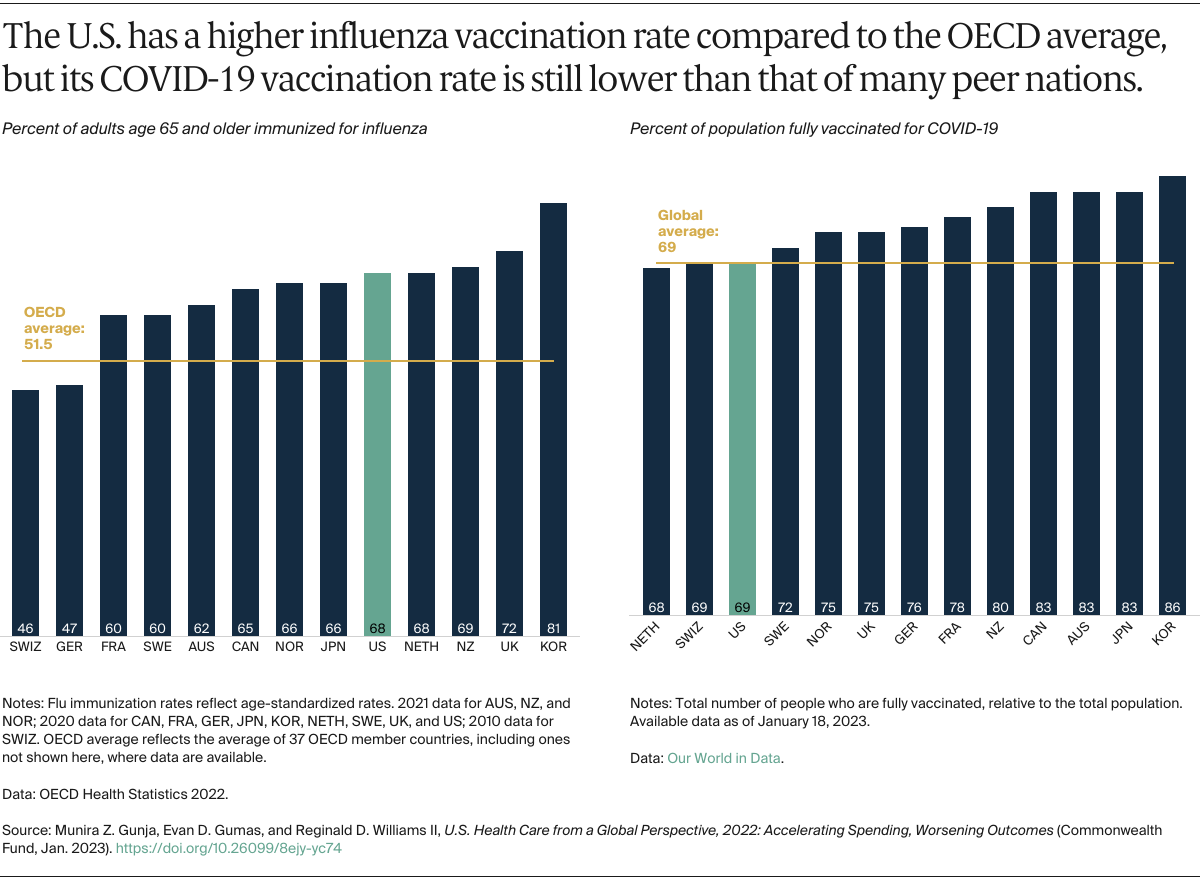
This analysis used data from Our World in Data, which compiles data from most countries and territories around the world across a range of measures. Data for confirmed COVID-19 deaths and COVID-19 vaccination rates were extracted in January 2023. A limitation of both data sets is that they only report confirmed deaths and reported vaccination rates, which Our World in Data notes can be underestimates. Full details on how indicators are defined, as well as country-level differences in data collection, are available from Our World in Data.25
Limitations of Our Analysis
The effects of the COVID-19 pandemic, including job loss and the postponement or forgoing of needed care, likely worsened many health outcomes.26 Therefore, some of our cross-country analyses should be interpreted with caution, as data for 2020 and beyond were not available for all countries or for every measure. As businesses and health care facilities continue to reopen and return to pre-COVID levels of operation, the health burdens individuals faced globally during the pandemic may continue to linger.
Another limitation of our study is that are we were unable to break out the data by race and ethnicity. Research has uncovered huge health disparities in the U.S., particularly for Black and Latino Americans.27 Efforts to collect data by race and ethnicity are needed on a global level to allow policymakers to not only make cross-country comparisons but also to see how health outcomes compare among vulnerable and historically neglected populations around the world.