Abstract
- Issue: Nearly all U.S. adults over 65 have some mental health coverage through Medicare. Whether that coverage is sufficient is in question. Comparing mental health care access and affordability for U.S. Medicare beneficiaries with that for older adults in peer nations could highlight coverage gaps and point to opportunities for improvement.
- Goals: To compare rates of self-reported diagnosed mental health problems, mental health burden, and financial hardship for adults 65 and over in the United States with those in 10 other high-income countries since the start of the COVID-19 pandemic.
- Methods: Analysis of findings from the 2021 Commonwealth Fund International Health Policy Survey of Older Adults.
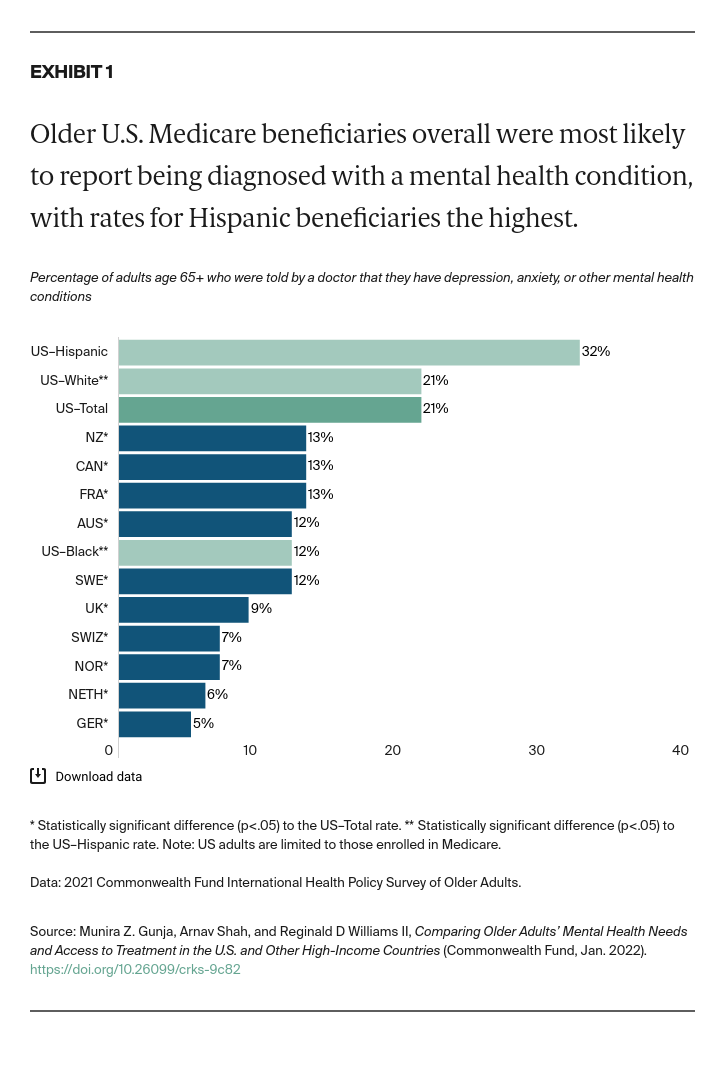
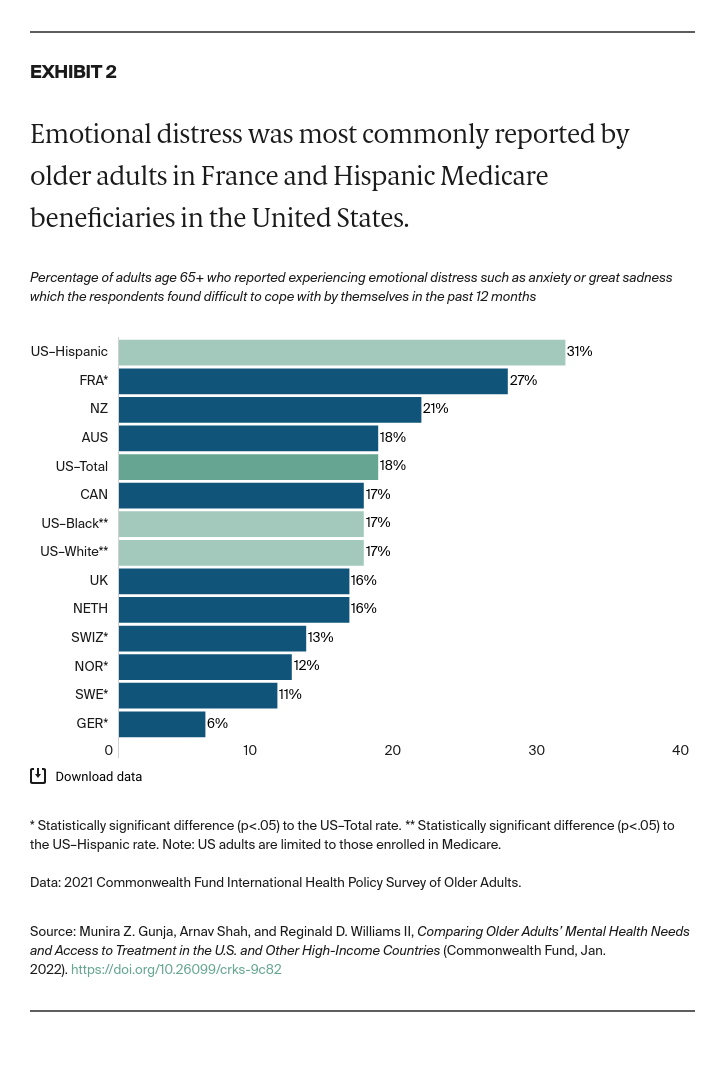
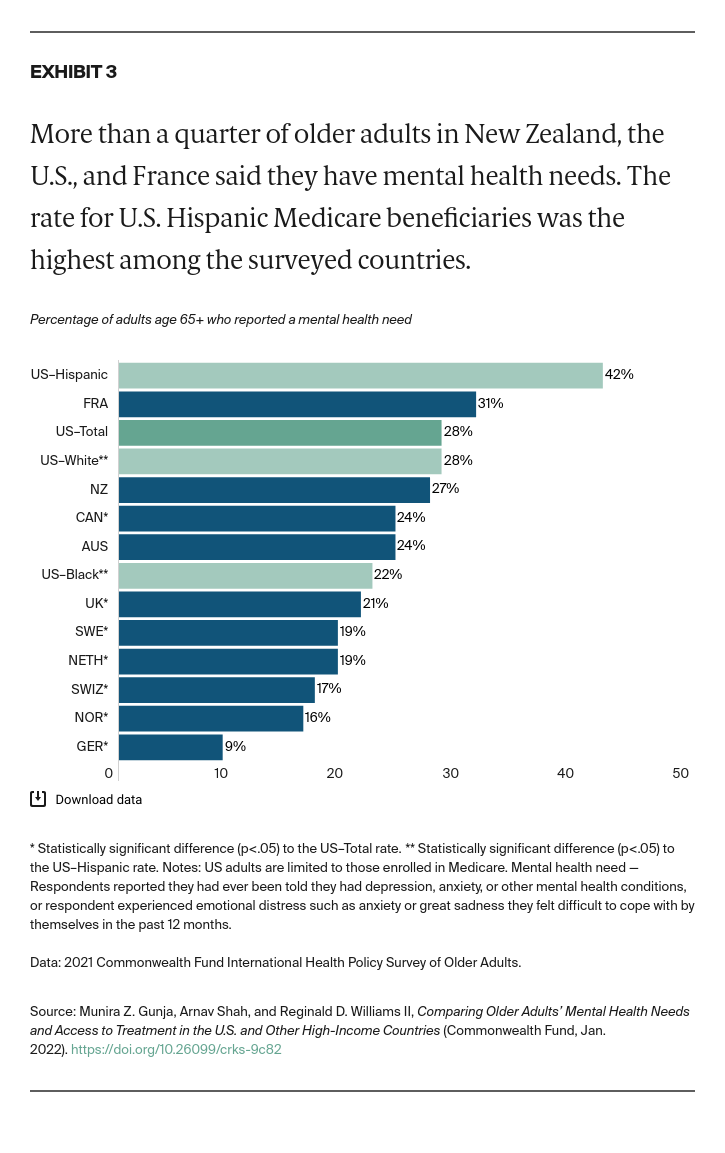
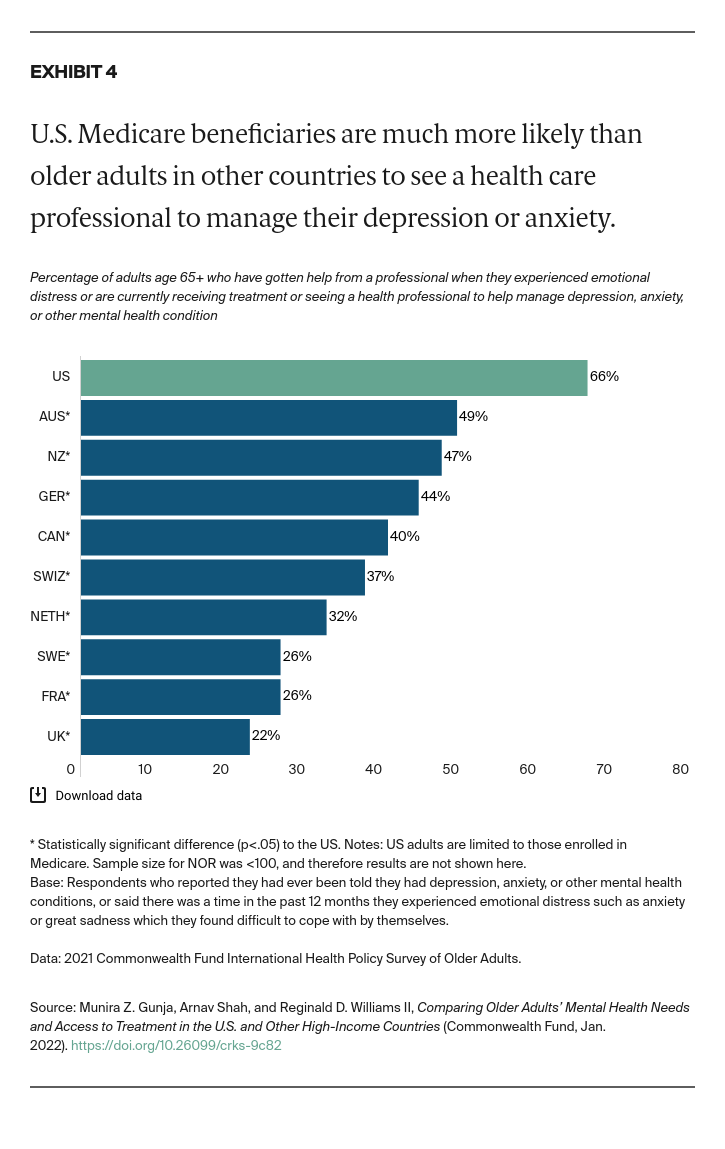
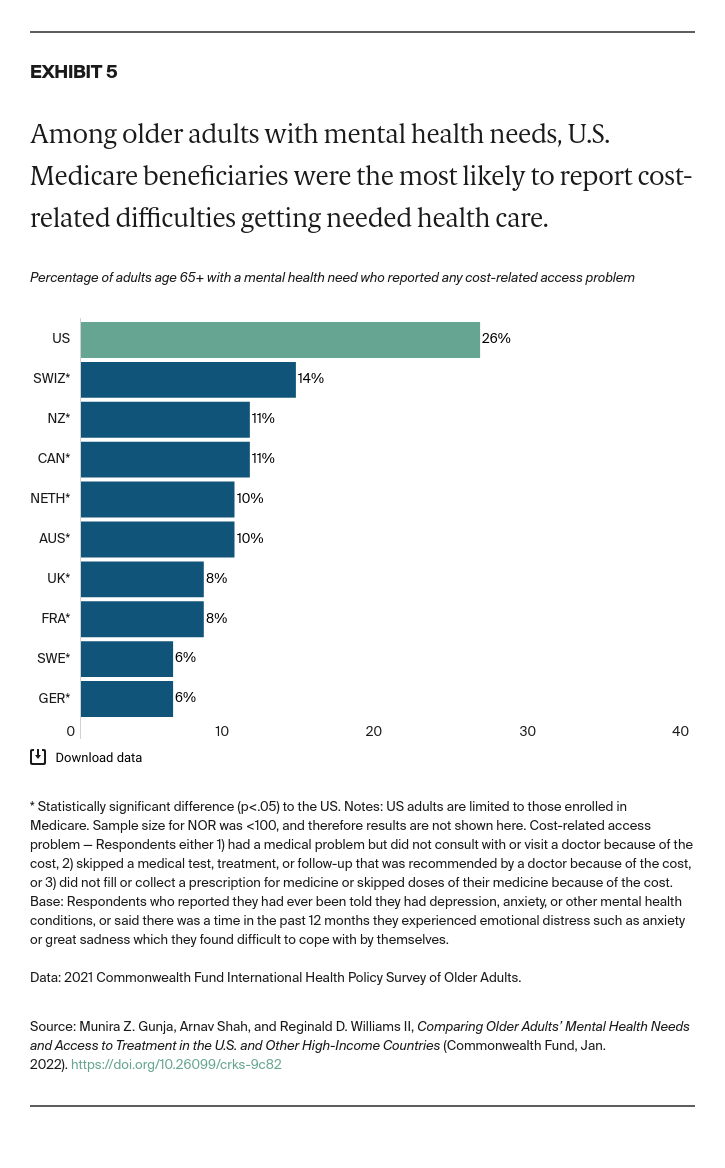
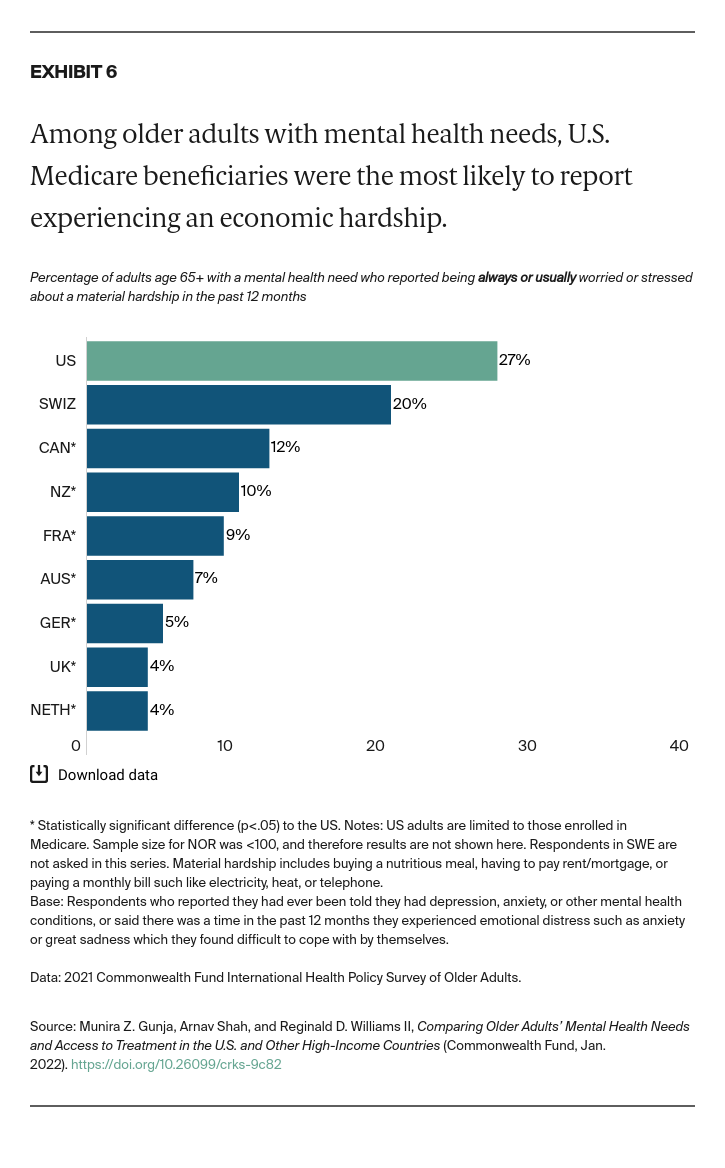
- Key Findings: Among older adults in the 11 countries, U.S. Medicare beneficiaries were the most likely to report being diagnosed with a mental health condition. The rate was highest for Hispanic/Latinx beneficiaries. U.S. respondents were also the most likely to report seeking care for their mental health condition, skipping needed care due to cost, and worrying about material hardship. Possible areas for U.S. reform include removing financial barriers to mental health services, addressing unmet social needs of individuals with mental health problems, and further investigating the pronounced disparities between older Hispanic/Latinx adults and other groups.
Introduction
Nearly all U.S. adults over age 65 have some mental health coverage through their enrollment in Medicare, which covers annual depression and substance use screenings, outpatient therapy, and counseling services, among other services.1 But is that coverage enough to ensure older Americans’ mental health needs are being met, especially as cases of depression and other mental health disorders have risen during the pandemic?2
Drawing on findings from a survey of more than 18,000 adults age 65 and older in 11 high-income countries, we compare Medicare beneficiaries in the United States with older adults in other high-income countries with regard to mental health burden, ability to access and afford needed mental health care, and experience of financial hardship.3 (When our sample size allows for it, we also show how these results compare for different races and ethnicities within the U.S.)
Conducted by the research firm SSRS and the Commonwealth Fund’s international partners, the survey was fielded between March and June 2021. It is the latest in the Commonwealth Fund’s series of International Health Policy Surveys, conducted annually to enable cross-national comparisons between the U.S. and other high-income countries.