Introduction
Maternal mortality rates are a key indicator of the health and well-being of a society. Yet this measure does not capture everything related to maternal health and well-being. It is also crucial to track:
- “Near miss” events that could have resulted in death.
- Severe maternal morbidity, defined by the U.S. Centers for Disease Control and Prevention as “unexpected outcomes of labor and delivery that result in significant short- or long-term consequences to a woman’s health.”
- Serious illnesses that occur during pregnancy, like ectopic pregnancy, and the postpartum period, like cardiomyopathy.
A richer understanding of maternal health before, during, and after childbirth is a foundation for developing safer, more effective approaches to maternal care. While maternal deaths in the United States number about 650 to 750 annually, severe maternal morbidity affects approximately 50,000 to 60,000 women each year, and the numbers are increasing. As with maternal deaths, many cases of maternal morbidity can be avoided.
This report describes the severity and breadth of the maternal morbidity crisis in the U.S. and shows why addressing it is critical to advancing maternal health equity. A companion to Maternal Mortality in the United States: A Primer, it is the latest in a series of Commonwealth Fund publications investigating the causes of poor maternal outcomes — including stark racial inequities — and identifying potential solutions.
Highlights
- Maternal morbidity is emerging as an important measure in efforts to prevent maternal mortality and address maternal health inequities.
- Each year, as many as 60,000 U.S. women are affected by severe maternal morbidity — unexpected outcomes of labor or delivery that have serious short- or long-term health impacts. In most instances, these outcomes could have been avoided with timely, appropriate care.
- Broadening the definition of severe maternal morbidity to also encompass serious illnesses during pregnancy and postpartum reveals the broader scope of the problem as well as the need for further measurement efforts and policy intervention.
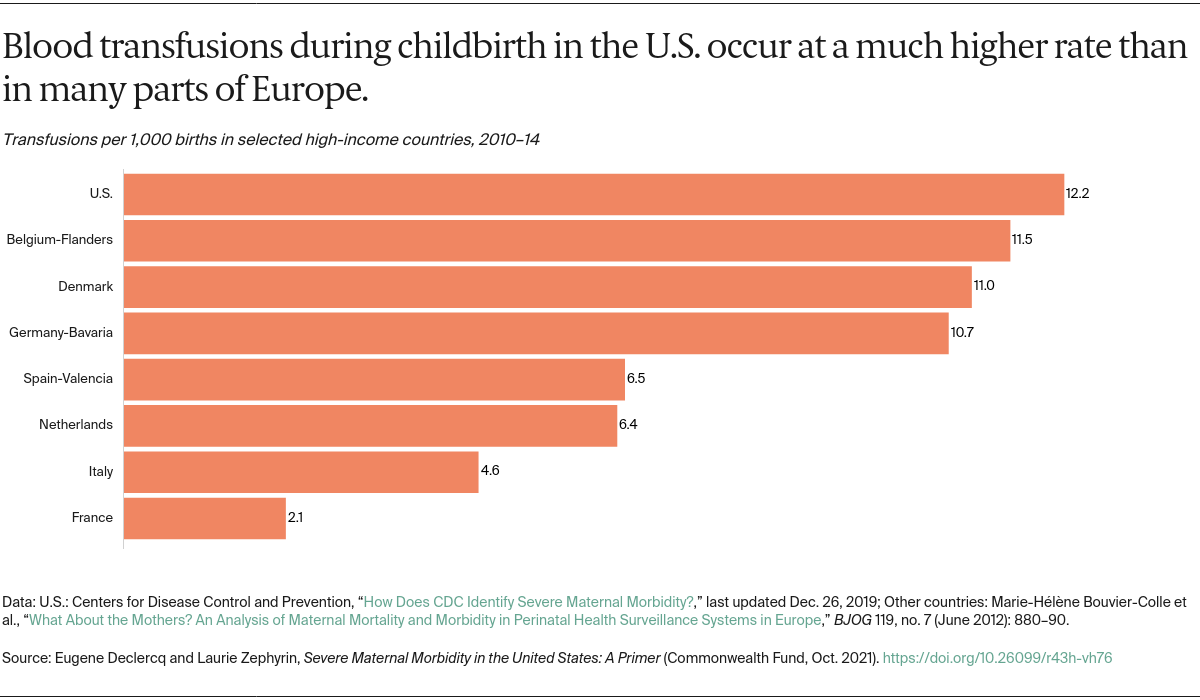
The U.S. Centers for Disease Control and Prevention (CDC) and the American College of Obstetricians and Gynecologists (ACOG) have offered detailed recommendations for monitoring and review of severe pregnancy and delivery complications. Both recommend facility-level, multidisciplinary review of all cases using a two-factor scoring system that identifies severe maternal morbidity by: 1) admission to the intensive care unit (ICU) and/or 2) transfusion of four or more units of blood products at any time from conception through 42 days postpartum. The scoring system, developed by Stacie Geller and colleagues, has been validated and can be used in real time in hospital settings, unlike administrative datasets currently used for population-level surveillance. To date, severe maternal morbidity reviews remain rare, having been implemented in individual facilities in California, and Illinois recently piloted a statewide operation through its regionalized perinatal system. In the future, severe morbidity reviews may increase as more hospital systems assess their experience with severe morbidity and states expand the scope of their maternal mortality reviews.