1. Lauren M. Rossen et al., “The Impact of the Pregnancy Checkbox and Misclassification on Maternal Mortality Trends in the United States, 1999–2017,” Vital and Health Statistics, series 3, no. 44 (National Center for Health Statistics, Jan. 2020); Marian F. MacDorman et al., “Recent Increases in the U.S. Maternal Mortality Rate: Disentangling Trends from Measurement Issues,” Obstetrics and Gynecology 128, no. 3 (Sept. 2016): 447–55; Building U.S. Capacity to Review and Prevent Maternal Deaths: Report from Nine Maternal Mortality Review Committees (Maternal Mortality Review Information Application and Review to Action, 2018); and Emily E. Petersen et al., “Vital Signs: Pregnancy-Related Deaths, United States, 2011–2015, and Strategies for Prevention, 13 States, 2013–2017,” Morbidity and Mortality Weekly Report 68, no. 18 (May 10, 2019): 423–29.
2. Commonwealth Fund International Health Policy Survey.
3. Roosa Tikkanen et al. (eds.), International Profiles of Health Care Systems 2020 (Commonwealth Fund, June 2020); and Stephen Morrissey et al., “International Health Care Systems,” New England Journal of Medicine 372, no. 1 (Jan. 1, 2015): 75–76.
4. Eugene Declercq and Laurie Zephyrin, Maternal Mortality in the United States: A Primer (Commonwealth Fund, forthcoming).
5. Declercq and Zephyrin, Maternal Mortality: Primer, forthcoming.
6. Declercq and Zephyrin, Maternal Mortality: Primer, forthcoming.
7. Global Burden of Disease 2015 Maternal Mortality Collaborators, “Global, Regional, and National Levels of Maternal Mortality, 1990–2015: A Systematic Analysis for the Global Burden of Disease Study 2015,” Lancet 388, no. 10053 (Oct. 8, 2016): 1775–812.
8. American College of Nurse-Midwives, Essential Facts About Midwives (ACNM, May 2019); World Health Organization, Nursing and Midwifery in the History of the World Health Organization 1948–2017 (WHO, 2017); Mary J. Renfrew et al., “Midwifery and Quality Care: Findings from a New Evidence-Informed Framework for Maternal and Newborn Care,” Lancet 384, no. 9948 (Sept. 20, 2014): 1129–45; and Jennifer E. Moore et al., Improving Maternal Health Access, Coverage, and Outcomes in Medicaid: A Resource for State Medicaid Agencies and Medicaid Managed Care Organizations (Institute for Medicaid Innovation, 2020).
9. Jane Sandall et al., “Midwife-Led Continuity Models Versus Other Models of Care for Childbearing Women,” Cochrane Database System Review 4 (Apr. 28, 2016): CD004667.
10. United Nations Population Fund, The State of World’s Midwifery 2014: A Universal Pathway. A Woman’s Right to Health. (UNFPA, 2014).
11. Renfrew et al., “Midwifery and Quality Care,” 2014.
12. Jesse S. Bushman, “The Role of Certified Nurse-Midwives and Certified Midwives in Ensuring Women’s Access to Skilled Maternity Care,” presentation, American College of Nurse-Midwives, Nov. 2015.
13. The American College of Nurse-Midwives estimates that approximately 60 percent of pregnancies are normal or low-risk. See Bushman, “Role of Certified Nurse-Midwives,” 2015. Other experts estimate that an even larger proportion of births, up to 90 percent, are considered uncomplicated. See UCSF Health, “High Risk Pregnancy,” n.d.
14. Martin Marshall, “A Precious Jewel — The Role of General Practice in the English NHS,” New England Journal of Medicine 372, no. 10 (Mar. 5, 2015): 893–97; and Ewout van Ginneken, “Perennial Health Care Reform — The Long Dutch Quest for Cost Control and Quality Improvement,” New England Journal of Medicine 373, no. 10 (Sept. 3, 2015): 885–89.
15. Dionne S. Kringos et al. (eds.), Building Primary Care in a Changing Europe (European Observatory on Health Systems and Policies, 2015).
16. Lianne Zondag, Franka Cadee, and Myrte de Geus, Midwifery in the Netherlands, 2017 (Royal Dutch Organization of Midwives, Jan. 2017); and Dorothy Shaw et al., “Drivers of Maternity Care in High-Income Countries: Can Health Systems Support Woman-Centred Care?,” Lancet 388, no.10057 (Nov. 5, 2016): 2282–95.
17. Marshall, “A Precious Jewel,” 2015.
18. American College of Nurse-Midwives, Ensuring Access to High Value Providers: ACNM Survey of Marketplace Insurers Regarding Coverage of Midwifery Services (ANCM, Sept. 2014); Marian F. MacDorman and Eugene Declercq, “Trends and Characteristics of United States Out-of-Hospital Births 2004–2014: New Information on Risk Status and Access to Care,” Birth 43, no. 2 (June 2016): 116–24.
19. Y. Tony Yang and Katy B. Kozhimannil, “Making a Case to Reduce Legal Impediments to Midwifery Practice in the United States,” Women’s Health Issues 25, no. 4 (July–Aug. 2015): 314–17.
20. World Health Organization et al., Postnatal Care for Mothers and Newborns: Highlights from the World Health Organization 2013 Guidelines (WHO et al., April 2015).
21. Christine MacArthur et al., “Effects of Redesigned Community Postnatal Care on Women’s Health 4 Months After Birth: A Cluster Randomised Controlled Trial,” Lancet 359, no. 9304 (2002): 378–85; Ian M. Paul et al., “A Randomized Trial of Single Home Nursing Visits vs. Office-Based Care After Nursery/Maternity Discharge: The Nurses for Infants Through Teaching and Assessment After the Nursery (NITTANY) Study,” Archives of Pediatric Adolescent Medicine 166, no. 3 (Mar. 2012): 263–70; and Kenneth A. Dodge et al., “Implementation and Randomized Controlled Trial Evaluation of Universal Postnatal Nurse Home Visiting,” American Journal of Public Health 104, no. S1 (Feb. 2014): S136–S143.
22. Kathy Gifford et al., Medicaid Coverage of Pregnancy and Perinatal Benefits: Results from a State Survey (Henry J. Kaiser Family Foundation, Apr. 2017).; and Alison Stuebe et al., “Extending Medicaid Coverage for Postpartum Moms,” Health Affairs Blog, May 6, 2019.
23. New Zealand Ministry of Health, “The First-Week Visit,” last updated June 30, 2015.
24. International Labor Organization, “Maternity Leave and Related Types of Leave,” in Maternity Protection Resource Package: From Aspiration to Reality for All (ILO, 2012).
25. Saraswathi Vedam et al., “Mapping Integration of Midwives Across the United States: Impact on Access, Equity, and Outcomes,” PLoS One 13, no. 2 (Feb. 21, 2018): e0192523.
26. Association of State and Territorial Health Officials, “COVID-19’s Impact on Pregnancy and Childbirth Policies,” ASTHO Experts Blog, Apr. 22, 2020; and Taylor Platt, States Implement Strategies to Safeguard Pregnant Women during the COVID-19 Pandemic (National Academy for State Health Policy, Apr. 20, 2020).
27. ANCM, Ensuring Access, 2014; and Moore et al., Improving Maternal Health Access, 2020.
28. Kirstie Coxon et al., “The Impact of the Coronavirus (COVID-19) Pandemic on Maternity Care in Europe,” Midwifery 88 (Sept. 2020): 102779; and WHO Europe, “Coronavirus and Pregnancy — Preserving Maternal Health Across the European Region,” WHO, June 30, 2020.
29. Tikkanen et al., International Profiles, 2020.
30. For example, many types of non-ACA-compliant plans, such as short-term plans or association health plans as well as some student health plans, don’t cover maternity benefits. Some young adults staying on a parent’s health plan have not had their maternity care costs covered, because the ACA only mandates maternity care coverage for primary beneficiaries, not for their children. In addition, the ACA’s 10 essential health benefits that insurers must cover, which include maternity care, apply only to individual marketplace insurance plans and small-group plans — but not employers with more than 50 workers.
31. Robin A. Cohen and Michael E. Martinez, Health Insurance Coverage: Early Release of Estimates from the National Health Interview Survey, 2013 (National Center for Health Statistics, June 2014).
32. Health Resources and Services Administration, The Maternal, Infant, and Early Childhood Home Visiting Program: Partnering with Parents to Help Children Succeed (HRSA, Apr. 2020).
33. WHO et al., Postnatal Care, 2015; and “ACOG Committee Opinion No. 736: Optimizing Postpartum Care,” Obstetrics and Gynecology 131, no. 5 (May 2018): e140–e150.
34. Medicaid and CHIP Payment and Access Commission (MACPAC), Medicaid’s Role in Financing Maternity Care (MACPAC, Jan. 2020); and Sarah H. Gordon et al., “Effects of Medicaid Expansion on Postpartum Coverage and Outpatient Utilization,” Health Affairs 39, no. 1 (Jan. 2020): 77–84.
35. Emily Eckert, “It’s Past Time to Provide Continuous Medicaid Coverage for One Year Postpartum,” Health Affairs Blog, Feb. 6, 2020; Laurie Zephyrin et al., “Increasing Postpartum Medicaid Coverage Could Reduce Maternal Deaths and Improve Outcomes,” To the Point (blog), Commonwealth Fund, Nov. 21, 2019; Review to Action and MMRIA, Report from Nine Maternal Mortality Review Committees (Review to Action, 2018); and Petersen et al., “Vital Signs,” 2019.
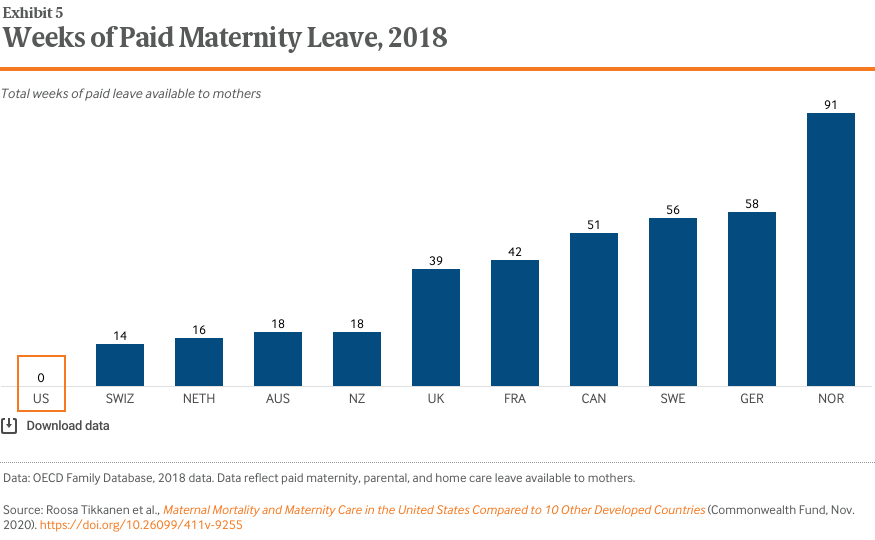
36. OECD Family Database, “Parental Leave Systems,” Aug. 2019.
37. Sarah A. Donovan, Paid Family Leave in the United States, Report R44835 (Congressional Research Service, updated May 29, 2019).
38. Judy Jou et al., “Paid Maternity Leave in the United States: Associations with Maternal and Infant Health,” Maternal and Child Health Journal 22, no. 2 (Feb. 2018): 216–25.
39. Donna L. Hoyert and Arialdi M. Miniño, “Maternal Mortality in the United States: Changes in Coding, Publication, and Data Release,” National Vital Statistics Report 69, no. 2 (Jan. 2020): 1–18.
40. Sandhya Raman, “COVID-19 Amplifies Racial Disparities in Maternal Health,” Roll Call, May 14, 2020; Black Women’s Maternal Health: A Multifaceted Approach to Addressing Persistent and Dire Health Disparities (National Partnership for Women & Families, Apr. 2018); Xenia Shih Bion, Efforts to Reduce Black Maternal Mortality Complicated by COVID-19 (California Health Care Foundation, Apr. 2020); and Yaphet Getachew et al., Beyond the Case Count: The Wide-Ranging Disparities of COVID-19 in the United States (Commonwealth Fund, Sept. 2020).
41. Marian Knight et al. (eds.), on behalf of MBRRACE-UK, Saving Lives, Improving Mothers’ Care: Lessons Learned to Inform Maternity Care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2015-17 (National Perinatal Epidemiology Unit, University of Oxford, Nov. 2019).
42. Morrissey et al., “International Health Care Systems,” 2015.