By Miriam Blümel and Reinhard Busse, Department of Health Care Management, Technische Universität Berlin
Health insurance is mandatory in Germany. Approximately 86 percent of the population is en-rolled in statutory health insurance, which provides inpatient, outpatient, mental health, and prescription drug coverage. Administration is handled by nongovernmental insurers known as sickness funds. Government has virtually no role in the direct delivery of health care. Sickness funds are financed through general wage contributions (14.6%) and a dedicated, supplementary contribution (1% of wages, on average), both shared by employers and workers. Copayments apply to inpatient services and drugs, and sickness funds offer a range of deductibles. Germans earning more than $68,000 can opt out of SHI and choose private health insurance instead. There are no government subsidies for private insurance.
Sections
How does universal health coverage work?
Chancellor Otto von Bismarck's Health Insurance Act of 1883 established the first social health insurance system in the world. At the beginning, health insurance coverage was restricted to blue-collar workers. In 1885, 10 percent of the population was insured and entitled to cash benefits in case of illness (50% of wages for a maximum of 13 weeks), death, or childbirth. While initially limited, coverage gradually expanded. The final step toward universal health coverage occurred in 2007, when health insurance, either statutory or private, was mandated for all citizens and permanent residents. Today’s system provides coverage for the entire population, along with a generous benefit package.
Health insurance is provided by two subsystems: statutory health insurance (SHI), consisting of competing, not-for-profit, nongovernmental health insurance plans known as sickness funds; and private health insurance.
Long-term care services are covered separately under Germany’s mandatory, statutory long-term care insurance (LTCI).
Unlike those in many other countries, sickness funds and private health insurers, as well as long-term care insurers, use the same providers. In other words, hospitals and physicians treat all patients regardless of whether they have SHI or private insurance.
Role of government: The German health care system is notable for the sharing of decision-making powers among the federal and state governments and self-regulated organizations of payers and providers (see exhibit).
Within Germany’s legal framework, the federal government has wide-ranging regulatory power over health care but is not directly involved in care delivery. The Federal Joint Committee, which is supervised by the Federal Ministry of Health, determines the services to be covered by sickness funds. To the extent possible, coverage decisions are based on evidence from comparative-effectiveness reviews and health technology (benefit-risk) assessments.
The Federal Joint Committee also sets quality measures for providers and regulates ambulatory care capacity (the number of SHI-contracted physicians practicing), using needs-based population–physician ratios.
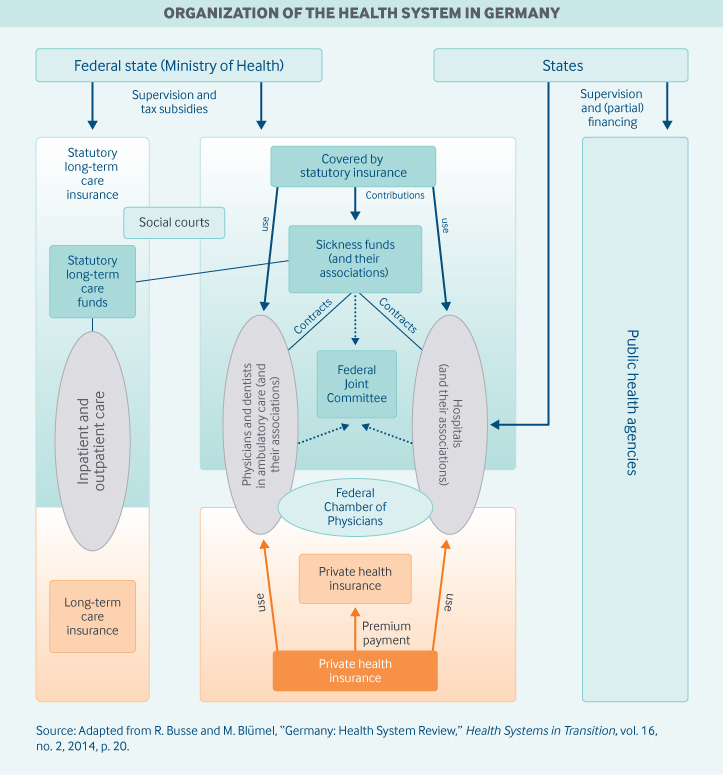
The Federal Joint Committee has 13 voting members: five representatives from associations of sickness funds, five from associations of providers, and three unaffiliated members. Five patient representatives have an advisory role but no vote. However, representatives of patient organizations have the right to participate in other decision-making bodies, including subcommittees of the Federal Joint Committee.
The Federal Association of Sickness Funds works with the Federal Association of Statutory Health Insurance Physicians and the German Hospital Federation to develop the ambulatory care fee schedule for sickness funds and the diagnosis-related group (DRG) catalog, which are then adopted by bilateral joint committees. Germany’s state governments also play an important administrative role. The 16 state governments determine hospital capacity and finance hospital investments. States also supervise public health services.
Regional associations of SHI-contracted physicians are required by law to guarantee the local availability of ambulatory services for all specialties in urban and rural areas. These regional associations also negotiate ambulatory physicians’ fee schedules with sickness funds.
Role of public health insurance: In 2017, total health expenditures made up 11.5 percent of the gross domestic product (GDP). Of this health spending, 74 percent was publicly funded, and most of that spending (57% of total) went toward SHI.
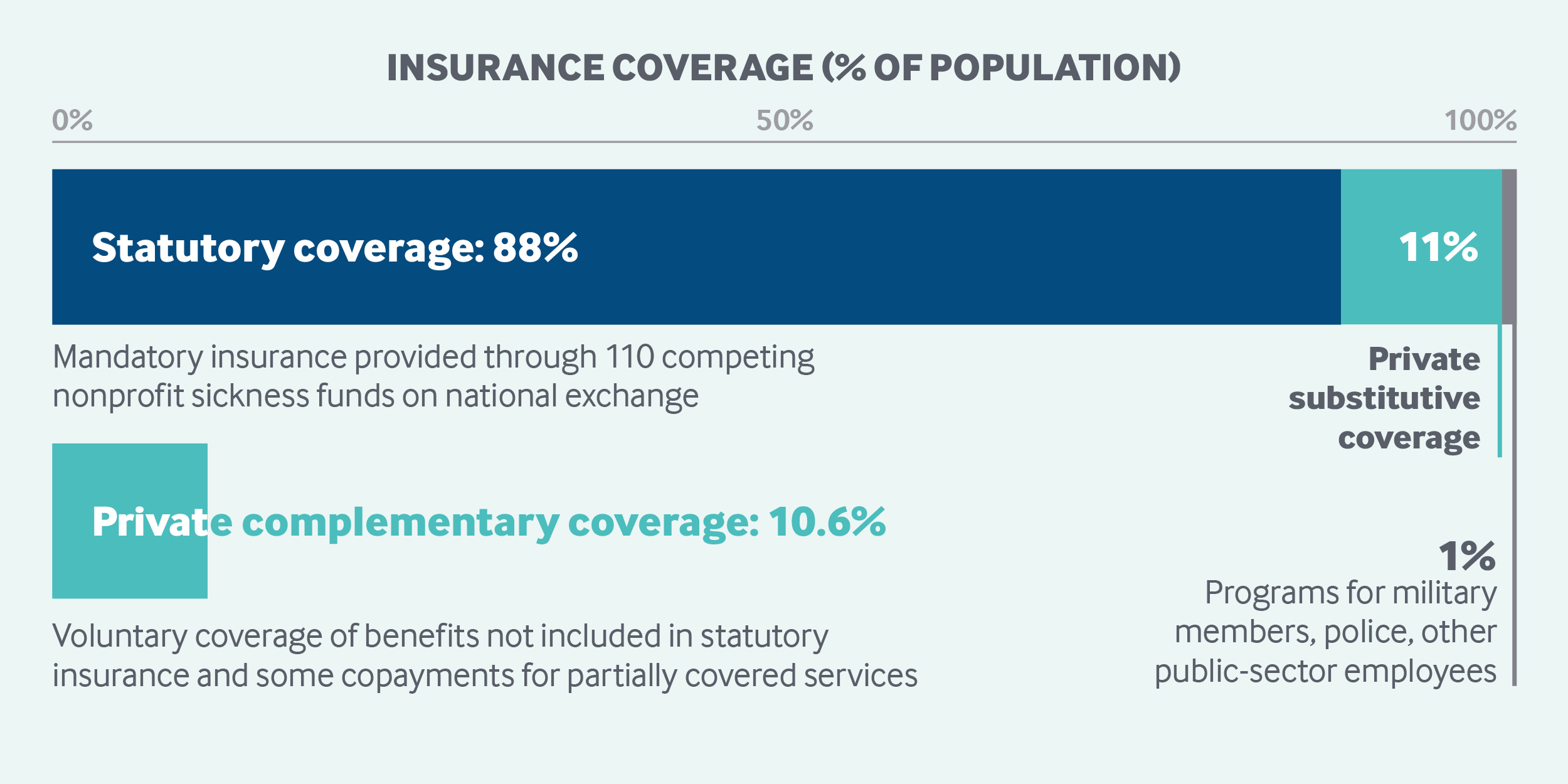
About 88 percent of the population receives primary coverage through sickness funds, and 11 percent through private insurance. There were 109 sickness funds in January 2019.1
As of 2019, all employed citizens (and other groups such as pensioners) earning less than EUR 60,750 (USD77,985) per year are mandatorily covered by SHI.2 Individuals whose gross wages exceed the threshold, as well as the self-employed who were previously covered by SHI, can elect to remain in the publicly financed scheme (as 75% do) or to purchase substitutive private health insurance. Civil servants are exempt from SHI; their private insurance costs are partly refunded by their employer. Military members, police, and other public-sector employees are covered under small programs that are separate from SHI. Visitors are not covered through German SHI. Refugees and undocumented immigrants are covered by social security in cases of acute illness and pain, as well as pregnancy and childbirth.
Sickness funds are financed through compulsory wage contributions levied as a percentage of gross wages up to a ceiling. Dependents (nonearning spouses and children) are covered free of charge. Since 2016, the legally set uniform contribution rate has been 14.6 percent of gross wages, shared equally by the employer and employees. As of 2019, earnings above EUR 54,450 (USD 69,897) per year are exempt from contribution.
The wage contributions are centrally pooled in a health fund (Gesundheitsfonds) and reallocated to individual sickness funds. A risk-adjusted capitation formula is used, accounting for age, sex, and morbidity from 80 chronic and serious illnesses.
In addition to compulsory wage contributions, a supplementary, income-dependent contribution is paid directly to the sickness funds, the rate of which is determined by the fund.3 For 2019, the average supplementary contribution rate is estimated at 1.0 percent.4
Role of private health insurance: In 2017, private health insurance accounted for 8.4 percent of total health expenditures.5 This includes substitutive coverage purchased by individuals who are exempt from or can opt out of SHI (such as higher-income individuals) as well as supplementary policies bought by sickness fund enrollees.
In 2017, 8.75 million people were covered through substitutive private health insurance.6 In June 2018, there were 41 substitutive private health insurance companies in Germany, of which 25 were for profit.7
The privately insured pay a risk-related premium, with separate premiums for dependents; risk is assessed only on entry, and contracts are based on lifetime underwriting. Private health insurance is especially attractive for young people with good incomes, as insurers may offer them contracts with a more extensive range of services and lower premiums.
For sickness fund enrollees, private insurance plays a mixed complementary and supplementary role, covering minor benefits not covered by SHI, including some copayments (like for dental care) and private hospital rooms.
Private health insurance is regulated by the Ministry of Health and the Federal Financial Supervisory Authority to ensure that the insured do not face large premium increases as they age and are not overburdened by premiums if their income decreases. The federal government determines provider fees under substitutive, complementary, and supplementary private insurance through a fee schedule. These fees tend to be higher than SHI fees. There are no government subsidies for private insurance.
Services covered: SHI covers the following:
- Preventive services, including regular dental checkups, child checkups, basic immunizations, chronic disease checkups, and cancer screenings at certain ages
- Inpatient and outpatient hospital care
- Physician services
- Mental health care
- Dental care
- Optometry
- Physical therapy
- Prescription drugs, except for those explicitly excluded by law (mainly so-called lifestyle drugs like appetite suppressants) and those excluded following an unfavorable benefit-risk assessment
- Medical aids
- Rehabilitation
- Hospice and palliative care
- Maternity care
- Sick leave compensation.
(See also the “ Long-term care and social supports” section for long-term care benefits.)
This broad framework for SHI benefits is defined by law; however, specifics are determined by the Federal Joint Committee.
Private benefit packages purchased by higher-income earners who opt out of SHI may be more extensive.
Cost-sharing and out-of-pocket spending: Out-of-pocket spending accounted for 13.5 percent of total health spending in 2017, and most individual spending went to nursing homes, pharmaceuticals, and medical aids.8
Copayments are determined by federal legislation and apply at the national level (see table below).
To compete for patients, sickness funds offer a range of deductibles and no-claims bonuses. Preventive services do not count toward the deductible, and there are no copayments for recommended preventive services (such as cancer screenings at certain ages).
Physicians who contract with sickness funds are not allowed to charge above the fee schedule for services in the SHI benefit catalogue. However, a list of individual health services outside the comprehensive range of coverage may be offered for a fee to patients paying out of pocket.
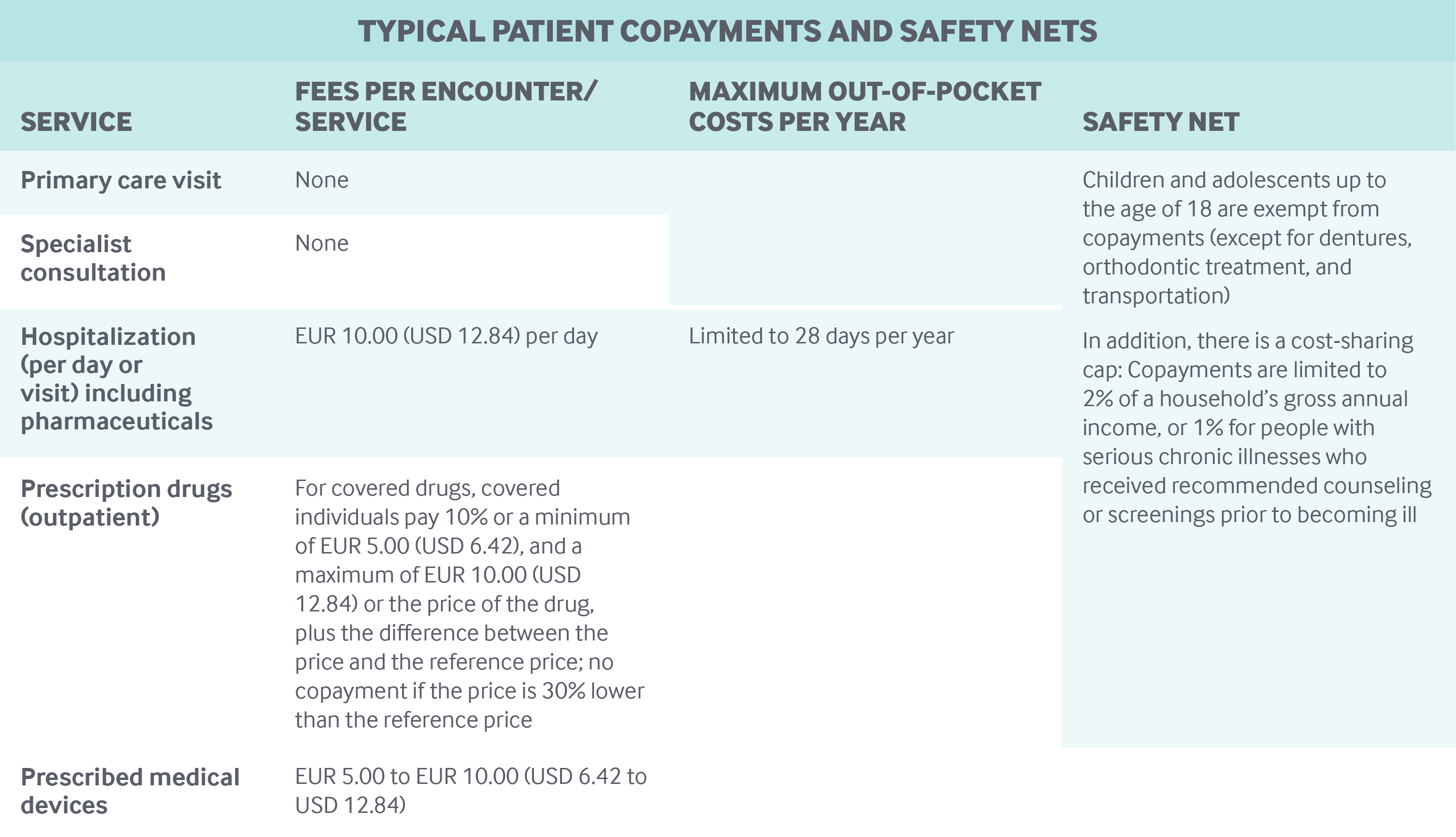
Safety nets: The unemployed contribute to SHI in proportion to their unemployment entitlements. For the long-term unemployed, the government contributes on their behalf. In addition, copayment caps and exemptions (see table above) help reduce the out-of-pocket burden on Germans.
How is the delivery system organized and how are providers paid?
Physician education and workforce: About 35 public universities and five private ones offer degrees in medicine. Studying at public universities is free, while private institutions sometimes require tuition fees ranging from EUR 6,000 (USD 7,702) to EUR 11,500 (USD 14,763) per semester. The minimum qualifications for a medical degree are determined at the federal level by the Licensing Regulations for Physicians, state laws, and individual university requirements. Specialization requirements are regulated and enforced by the medical chambers within each state.
Primary and outpatient specialist care: General practitioners (GPs) and specialists in ambulatory care typically work in their own private practices—around 56 percent in solo practice and 33 percent in dual practices. In 2017, there were about 2,500 multispecialty clinics, where some 18,000 of Germany’s ambulatory care physicians (11%) work. Most physicians working in multispecialty clinics are salaried employees. Some specialized outpatient care is provided by hospital specialists, including treatment of rare, severe, or progressive diseases as well as highly specialized procedures.
The total number of ambulatory care physicians and psychotherapists is more than 170,000.9 In 2017, family physicians, including GPs, internists, and pediatricians, accounted for 45 percent of self-employed, SHI-contracted ambulatory care physicians (57,600 of roughly 129,000), while 55 percent (71,400) were specialists.
Most physicians employ medical assistants, while other nonphysicians (such as physiotherapists) have their own premises. Advanced practice nurses have not yet prevailed in primary care; however, there are an increasing number of medical assistants who complete further training as care managers.
Individuals have free choice among GPs and specialists. Registration with a family physician is not required, and GPs have no formal gatekeeping function. However, sickness funds are required to offer members the option of enrolling in a family physician care model, which has been shown to provide better services than traditional care approaches and often provides incentives for complying with gatekeeping rules.
Under SHI, GPs and specialists are generally reimbursed on a fee-for-service (FFS) basis according to a uniform fee schedule that is negotiated between sickness funds and regional associations of physicians. The law requires SHI-contracted ambulatory physicians to be members of these regional associations, which act as financial intermediaries between physicians and sickness funds and are responsible for coordinating care requirements within their region.
The associations receive monies from sickness funds in the form of annual capitations. The physicians then bill the associations according to the SHI fee schedule. However, physician payments are limited to a predefined quarterly maximum number of patients per practice and reimbursement points per patient, setting quarterly thresholds for the number of patients and of treatments per patient for which a physician can be reimbursed. If physicians exceed the quarterly thresholds, they are paid considerably less for any additional services provided. This can lead physicians to postpone nonurgent patient visits once they reach the thresholds, which means patients may have longer appointments wait times at the end of each quarter.
For private patients, GPs and specialists are also paid on a fee-for-service basis, but private tariffs are usually higher than the tariffs in the SHI fee schedule.
The average SHI reimbursement for a family physician is more than EUR 200,000 (USD 256,739) per year. This must cover the costs of operating a practice, including personnel, etc. Physicians may also earn income from privately insured patients.
The average SHI reimbursement for ambulatory care specialists is about the same as for GPs. But reimbursement varies widely across specialties, depending on the specialty, from EUR 77,000 (USD 98,845) for a psychotherapist to EUR 367,000 (USD 471,117) for a radiologist, not including private health insurance reimbursements and direct patient payments.10
Pay-for-performance has not yet been established. Financial incentives for care coordination can be part of integrated-care contracts, but are not routinely implemented. The only regular financial incentive that GPs receive is a fixed annual bonus (EUR120, or USD154, in 2016) for patients enrolled in a disease management program, in which physicians provide patient training and document patient data. Bundled payments are not common in primary care. But a regional shared-savings initiative, called Healthy Kinzigtal (named for a valley in southwest Germany), offers primary care physicians and other providers financial incentives for integrating care across providers and services.
Administrative mechanisms for direct patient payments to providers: Copayments or payments for services not included in the SHI benefit package are paid directly to the provider. In cases of private health insurance, patients pay up front and submit claims to the insurance company for reimbursement.
After-hours care: After-hours care is organized by the regional associations to ensure access to ambulatory care around the clock. After-hours care assistance is available mainly through a nationwide telephone hotline. However, physicians are obliged to provide after-hours care in their practices, with differing regional regulations. In some areas, such as Berlin), after-hours care has been delegated to hospitals. The patient is given a report of the visit afterwards to hand to his or her GP.
There is also a tight network of emergency care providers (under the responsibility of the municipalities). Payment for ambulatory after-hours care is based on fee schedules, with differences in the amount of reimbursement by SHI and private health insurance.
Hospitals: Public hospitals make up about half of all beds, while private not-for-profits account for about a third. The number of private, for-profit hospitals has been growing in recent years (now accounting for about one-sixth of all beds). All hospitals are staffed principally by salaried physicians. Physicians in hospitals (similar to U.S. hospitalists) are typically not allowed to treat outpatients, but exceptions are made if necessary care cannot be provided by office-based specialists. Senior doctors can treat privately insured patients on an FFS basis. Hospitals can also provide certain highly specialized services on an outpatient basis.
Inpatient care is paid per admission through a system of DRGs, which are revised annually. Currently, there are around 1,300 DRG categories. DRGs cover all services and all physician costs. Highly specialized and expensive services like chemotherapy, as well as new technologies, can be reimbursed through supplementary fees. Other payment systems like pay-for-performance or bundled payments have yet to be implemented in hospitals.
Mental health care: Acute psychiatric inpatient care is provided largely by psychiatric wards in general (acute) hospitals. The number of hospitals providing care only for patients with psychiatric and/or neurological illnesses is low.
In the ambulatory care sector, there were about 38,000 office-based psychiatrists, neurologists, and psychotherapists in 2017.11 Qualified GPs can provide basic psychosomatic services. Ambulatory psychiatrists also coordinate a set of SHI-financed benefits called sociotherapeutic care (which requires referral by a GP), intended to encourage the chronically mentally ill to access needed care and to avoid unnecessary hospitalizations. To further promote outpatient care for psychiatric patients (particularly in rural areas with a low density of ambulatory psychiatrists), hospitals can be authorized to offer treatment in outpatient psychiatric departments.
Long-term care and social supports: Statutory LTCI is mandatory. People typically get statutory LTCI from the same insurers that provide SHI. Employees share the contribution rate of 3.05 percent of gross salary with their employers; people without children pay an additional 0.25 percent.
Everybody with a physical or mental illness or disability (who has contributed for at least two years) can apply for LTCI benefits, which are:
- Dependent on an evaluation of individual care needs by the SHI Medical Review Board, which leads either to a denial of benefits or to an assignment to one of five levels of care
- Limited to certain maximum amounts, depending on the level of care.
Beneficiaries can choose between free or discounted long-term care services and cash payments. Around a quarter of LTCI expenditures go toward cash payments. Both home and institutional care are provided almost exclusively by private not-for-profit and for-profit providers.
As benefits usually cover approximately only 50 percent of institutional care costs, people are advised to buy supplementary private LTCI. In 2016, around 3.4 million Germans with SHI and private health insurance also had supplementary private LTCI.
As a separate public benefit, family caregivers get financial support through continuing payment of up to 50 percent of care costs.
Of the approximately 2.9 million recipients of long-term care in 2015, 48 percent were cared for at home by relatives, 24 percent received home care supplied by ambulatory care service providers, and 27 percent were treated as inpatients in nursing homes.
Hospice care is partly covered by LTCI if the SHI Medical Review Board has determined a care level. Medical services or palliative care in a hospice are covered by SHI. The number of inpatient facilities in hospice care has grown significantly over the past 15 years, to 235 hospices and 304 palliative care wards nationwide in spring 2016.12
What are the major strategies to ensure quality of care?
Quality of care is addressed through a range of measures broadly defined by law and in more detail by the Federal Joint Committee. The Institute for Quality Assurance and Transparency (IQTiG) is responsible for measuring and reporting on quality of care and provider performance on behalf of the Federal Joint Committee. In addition, the institute develops criteria for evaluating certificates and quality targets and ensures that the published results are comprehensible to the public. All hospitals are required to publish findings on selected indicators, as defined by the IQTiG, to enable hospital comparisons. There is a mandatory quality reporting system for the roughly 1,600 acute-care hospitals, in which data of 290 publicized process and outcome indicators across 30 treatment areas are collected. Based on these data, sickness funds and the White List (Weisse Liste), a nonpartisan online tool, report outcomes to help patients choose hospitals. Indicators for quality-related hospital accreditation and payment are currently being developed.
Nursing homes and home care agencies are assessed by the regional SHI Medical Review Boards for, among other things, care deficits. The results of these quality checks are published in transparency reports. In addition, scores in nursing care are created based on these checks and surveys of nursing home residents and employees.
Structural quality is further assured by the requirement that providers have a quality management system, by the stipulation that all physicians continue their medical education, and by health technology assessments for drugs and procedures. For instance, all new diagnostic and therapeutic procedures applied in ambulatory care must receive a positive evaluation for benefit and efficiency before they can be reimbursed by sickness funds. In addition, the Institute for Quality and Efficiency in Health Care (IQWiG), an independent scientific institute, is legally charged with evaluating the cost-effectiveness of drugs with added therapeutic benefits.
Although there is no revalidation requirement for physicians, many institutions and health service providers include complaint management systems as part of their quality management programs. This system became obligatory for hospitals in 2013. At the state level, professional providers’ organizations are urged to establish complaint systems and arbitration boards for the extrajudicial resolution of medical malpractice claims.
The Robert Koch Institute, a governmental agency subordinate to the Federal Ministry of Health and responsible for the control of infectious diseases and for health reporting, has conducted national patient surveys and published epidemiological, public health, and health care data. Disease registries for specific diseases, such as certain cancers, are usually organized regionally. As part of the National Cancer Plan, the federal government passed a bill that mandated implementation of standardized cancer registries in all states by 2018 to improve the quality of cancer care. Full implementation, however, has yet to occur.
Disease management programs ensure quality of care for people with chronic illness. These programs are modeled on evidence-based treatment recommendations, with mandatory documentation and quality assurance.
Nonbinding clinical guidelines are produced by the Physicians’ Agency for Quality in Medicine and other professional societies.
What is being done to reduce disparities?
Compared to percentages in other European countries, the share of population reporting an unmet need for medical care is very low (0.3%), ranging between 0.8 percent in the lowest income quintile and 0.1 percent in the highest income quintile in 2017.13 This suggests good access with few disparities.
The Health Monitor (Gesundheitsmonitor) was a national initiative of not-for-profit organizations and sickness funds. To assess the performance of the health care system, it regularly conducted studies from the patient perspective—for example, on the availability of information, experiences with health care, and the progress of health system reforms. The Health Monitor, which last conducted a study in 2016, ceased to exist after 15 years. A comparable survey on health access has not been provided.
Strategies to reduce health disparities are delegated mainly to public health services, and the levels at which they are carried out differ among states. Health disparities are implicitly mentioned in the national health targets. A network of more than 120 health-related institutions, including sickness funds and their associations, promotes the health of the socially deprived.14 Primary preventive care is mandatory by law for sickness funds; detailed regulations are delegated to the Federal Association of Sickness Funds, which has developed guidelines regarding need, target groups, and access, as well as procedure and methods. Sickness funds support 22,000 health-related programs in nurseries, schools, and other setting.15
What is being done to promote delivery system integration and care coordination?
Many efforts to improve care coordination have been implemented; for example, sickness funds offer integrated care contracts and disease management programs for chronic illnesses to improve care for chronically ill patients and to improve coordination among providers in the ambulatory sector. In December 2017, 9,173 registered disease management programs for six indications had enrolled about 6.8 million patients (more than 9% of all the SHI-insured).16 There is no pooling of funding streams by the health and social care sectors.
Since 2016, the Innovation Fund has been promoting new forms of cross-sectoral and integrated care (also for vulnerable groups) with an annual funding of EUR300 million, or USD382 million (including EUR75 million, or USD95 million, for evaluation and health services research). Funds are awarded through an application process overseen by the Federal Joint Committee.17 So far, the fund has sponsored care models in structurally weak and rural regions and care models using telehealth.
What is the status of electronic health records?
Since 2015, electronic medical chip cards have been used nationwide by all the SHI-insured; they encode information including the person’s name, address, date of birth, and sickness fund, along with details of insurance coverage and the person’s status regarding supplementary charges.18 Patients can decide whether they want clinical data, such as on medications, to be stored and whether these are to be passed on to their physician.
In 2015, Parliament passed a law for secure digital communications and health care applications; the E-Health Act provides concrete deadlines for implementing infrastructure and electronic applications (such as documentation of willingness to donate organs) and introduces incentives and sanctions if schedules are not adhered to.
SHI physicians receive additional fees for sharing electronic medical reports with other providers (since 2016–2017), collecting and documenting emergency records (since 2018), and managing and reviewing basic insurance claims data online. In the future, SHI physicians who do not participate in online review of the basic insurance claims data will receive reduced remuneration.
Furthermore, to ensure greater safety in drug therapy, patients who use at least three prescribed drugs simultaneously will receive an individualized medication plan. In the medium term, this medication plan will be included in the electronic medical record.19
How are costs contained?
Recently, there has been a shift away from reliance on overall budgets for ambulatory physicians and hospitals and collective regional prescription caps for physicians, toward an emphasis on quality and efficiency. The Hospital Care Structure Reform Act of 2016 aims not only to link hospital payments to good service quality but also to reduce payments for low-value services. Currently, the IQTiG works on preparing appropriate concepts and recommendations for the Federal Joint Committee.
To enhance competition, some purchasing power has been handed over to the individual sickness funds instead of relying on collective contracts with regional associations. For example, the funds can now selectively negotiate integrated-care contracts with providers and negotiate rebates with pharmaceutical companies.
All drugs, both patented and generic, are placed into groups with a reference price serving as a maximum level for reimbursement, unless an added medical benefit can be demonstrated. For new drugs with added benefit (as evaluated by IQWiG and decided on by the Federal Joint Committee), the Federal Association of Sickness Funds negotiates a reimbursement price, based on the manufacturer’s price, that is applied to all patients. In addition, rebates are negotiated between individual sickness funds and pharmaceutical manufacturers to lower prices below the reference price.
What major innovations and reforms have recently been introduced?
After a period of active health reform in several areas between 2012 and 2016, new reform debates and proposals stagnated until spring 2018. One of the reasons is that after the federal elections in September 2017, it took six months of difficult talks and political insecurity to again form a grand coalition between political parties (Christian Democrats and Social Democrats). The first new bill introduced in 2018 (the SHI-Contribution Relief Law, or GKV-Versichertenentlastungsgesetz) aims to reduce the mandatory contributions that individuals in SHI pay every month.20 While the general contribution of 14.6 percent has been equally shared between employers and employees since 2015, the supplementary contribution is paid by employees only. The law plans to reinstate the equal split of general and supplementary contributions between employers and employees. Furthermore, the law stipulates halving the reference amount used to calculate the minimum contribution for the self-employed insured. Until now, independent of their actual income, the self-employed have paid a contribution based on expected minimum income of EUR 221 (USD 284) per month. This is unmanageable for a large proportion of small-business owners and increases their risk of having no health insurance.21
Furthermore, the Ministry of Health has recently issued a decree on minimum staffing requirements for nurses in hospitals. The maximum number of patients per nurse has been defined for hospital units where nursing staff is particularly needed — intensive care, geriatric, cardiology, and trauma surgery — to guarantee patient safety. The regulation went into effect January 2019. To further expand the capacities of nurses in hospitals and in long-term care and to reform salaries and working conditions for nurses, the Nursing Staff Strengthening Act was enacted in September 2018.22

