Research indicates that an estimated 20 percent of health outcomes are linked to medical care; the remaining 80 percent stem from socioeconomic, environmental, and behavioral factors referred to as social drivers of health (DOH). These factors — such as homelessness, food insecurity, and exposure to intimate partner violence — are associated with chronic illness, mental health issues, acute hospitalizations, and high health care costs and disproportionately impact communities of color.
The Biden administration has signaled its commitment to addressing DOH needs for patients with the recent release of a playbook for improving health-related social needs in communities. Over the past two years, the Centers for Medicare and Medicaid Services (CMS) has taken steps to address DOH by establishing standard definitions and adopting the first-ever DOH measures in federal health care programs that affect millions of Medicare and Medicaid beneficiaries. Specifically, CMS has:
- Approved the first DOH measures in the history of Medicare, starting with two value-based programs, the Merit-Based Incentive Payment System and the Hospital Inpatient Quality Reporting Program. The evidence-based measures call for clinicians to screen patients on drivers of health and report the percent of beneficiaries screened and the percent that screened positive for social needs. CMS has submitted or adopted these measures in six other federal quality or payment programs. Further, in the proposed 2023 physician fee schedule, CMS introduced the first DOH measure focused on connecting patients who screen positive to interventions or resources.
- Embraced the term “drivers of health” consistent with research that people — across race, gender, politics, and geography — vehemently reject the phrase “social determinants of health” as demeaning and confusing. In its 2023 Medicare physician fee schedule, CMS stated that it would “utilize ‘drivers of health’ terminology to minimize potential misinterpretation or negative connotation.”
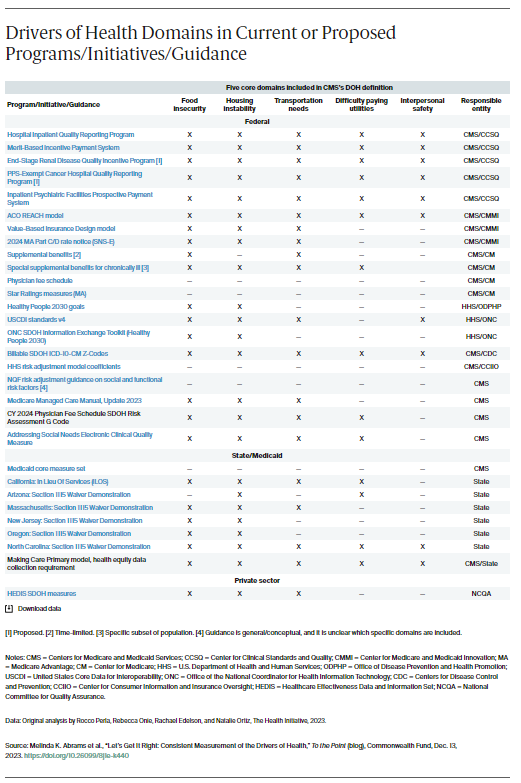
- Provided a standard definition of DOH by specifying five core domains: food insecurity, housing instability, transportation needs, difficulty paying utilities, and interpersonal safety. CMS selected these domains based on criteria including strong evidence showing the correlation between the five areas and patient health outcomes and the benefits of specific interventions and the ability to assess these domains in multiple health care settings. The domains also reflect beneficiaries’ greatest needs, were elevated by CMS’s technical expert panel, and received strong support from physicians and other stakeholders.
- Outlined measurement and reporting specifications for the five DOH domains. CMS encouraged the use of established, evidence-based screening instruments and provided detailed guidance on reporting requirements (e.g., numerators, denominators, exclusion criteria), which can facilitate consistent collection and reporting across Medicare and Medicaid.
Focusing on Implementation and Consistency
These steps have accelerated efforts to address the drivers of health and advance equity, but implementation has lagged. CMS defined and approved five key areas of social needs but most federal, state, and private sector programs only screen for or address a subset of those needs. Skipping any of these five critical areas could mean that people will not be connected to needed services. In addition, a recent analysis found inconsistency in the DOH definition across federal programs, state initiatives, and the private sector (see table).
We are at an important juncture in the field of quality measurement and should learn from past inefficiencies. Over the past 25 years, the clinical quality measurement movement generated thousands of measures with countless iterations. CMS now invests in large, multistakeholder coalitions to negotiate, debate, and reach consensus on consistent selection and reporting of quality measures across all value-based programs and payers (i.e., Medicare, Medicaid, Affordable Care Act marketplaces, commercial). The lack of alignment on measures has contributed to increased administrative costs and burden on providers and patients.
We have an opportunity at this early stage to press for consistency in the DOH domains measured in federal, state, and private sector programs. More consistent and routine collection will help providers and CMS track factors that influence people’s health and improve coordination among providers and between clinical and social service providers. Without this consistency, there is significant risk of care fragmentation and data quality issues — as well as frustrated clinicians, patients, and health plans — that may impede efforts to improve health outcomes, reduce disparities, and lower costs.
Looking Ahead
CMS could incorporate DOH measures into its proposed agencywide initiative called the Universal Foundation, which seeks to align quality measures across its 20 value-based programs that serve more than 150 million Americans. The agency also could ensure coordination with closely related electronic measurement efforts across the Department of Health and Human Services (HHS). For example, the HHS Office of the National Coordinator, which promotes interoperability standards for sharing electronic health information, recently proposed data capture for only four of the five DOH domains. Similarly, CMS’s latest effort to update electronic measures to address social needs could align with the new DOH measures by including all five domains; the current proposal excludes interpersonal safety. Since most Medicare and Medicaid beneficiaries obtain care through private health plans, CMS could incentivize plans to provide DOH-related benefits through regulation, guidance, and requests for proposals. All this could be supported and accelerated via the recently announced SDOH Data Working Group within the Executive Office of the President.
HHS and CMS have an unprecedented opportunity to standardize measurement, which could highlight the impact of DOH on health outcomes and help providers address the drivers that affect health care utilization, cost, and disparities. Consistent implementation of DOH measures represents an historic shift in national efforts to align collective resources, promote equitable health outcomes, and improve the health of millions of Americans.