Synopsis
Low-income adults in Kentucky and Arkansas, which both expanded Medicaid eligibility under the Affordable Care Act, were more likely to be insured and less likely to have problems paying medical bills or affording prescriptions than low-income adults in Texas, which did not expand Medicaid.
The Issue
The Affordable Care Act (ACA) gives states the option to expand Medicaid eligibility to all adults with incomes under 138 percent of the federal poverty level (about $16,000 for an individual or $33,000 for a family of four). So far, 30 states and the District of Columbia have chosen to do so. Most have taken a traditional approach to expanding Medicaid, but several have elected the “private option”—using Medicaid funds to purchase private insurance through the federal and state marketplaces. This Commonwealth Fund–supported article in Health Affairs examines the experiences of low-income adults during the first year of the ACA Medicaid expansion in three states that adopted different strategies: Kentucky, which expanded traditional Medicaid coverage; Arkansas, which used the private option; and Texas, which did not expand Medicaid.
Findings suggest that deciding whether or not to expand [Medicaid] matters much more than deciding how to expand.
Key Findings
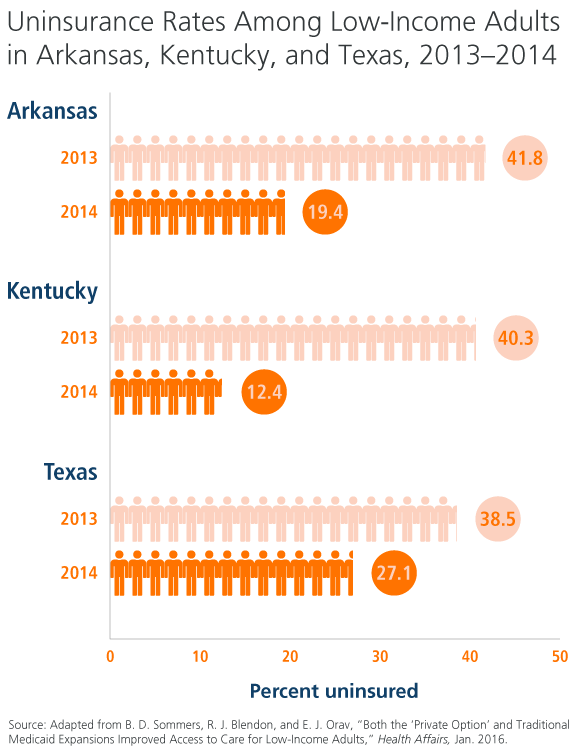
- The uninsured rate in Kentucky and Arkansas dropped 14 percentage points more than in Texas between 2013 and 2014.
- In 2013, the uninsured rate was about 40 percent in all three states. But by 2014, it had dropped to 19 percent in Arkansas and 12 percent in Kentucky, while falling to 27 percent in Texas. Even in nonexpansion states like Texas, the streamlined Medicaid application process and the publicity surrounding the ACA helped increase coverage among uninsured populations, the authors point out. Moreover, in all states, low-income people living between 100 percent and 138 percent of the federal poverty level are eligible for subsidies when buying coverage in the marketplaces.
- In Kentucky and Arkansas, the share of adults who said they were struggling to pay medical bills fell by nearly 9 percentage points more than in Texas. The share of those reporting not filling a prescription because of the cost fell nearly 10 percentage points more in the expansion states.
- Low-income adults in Kentucky experienced an even larger decline in medical bill problems compared with those in Arkansas, suggesting that Medicaid provides greater financial protection than private coverage, even with cost-sharing subsidies.
- The percentage of people visiting emergency departments (EDs) because they could not get a timely appointment in a physician’s office increased nearly 5 percentage points more in Kentucky and Arkansas compared with Texas. However, the share of adults in those two states reporting that the ED was their usual source of care dropped by 5 percentage points.
- Among adults with chronic illnesses like high blood pressure or diabetes, the share who reported receiving regular care for those conditions increased nearly 12 percentage points more in the expansion states than in Texas.
The Big Picture
While there has been debate regarding the merits of the two Medicaid expansion approaches, this study found no significant differences (other than trouble paying medical bills) between Kentucky’s traditional approach and Arkansas’s private option. “[O]ur findings suggest that deciding whether or not to expand matters much more than deciding how to expand,” the authors write. Both models appear to be promising strategies to improving access to care among low-income adults. The authors note that additional research will be critical for evaluating the ACA’s long-term impact on this population.
About the Study
Researchers surveyed low-income adults in Kentucky, Arkansas, and Texas from November to December 2013, and again one year later. The survey asked people about health insurance; access to care (e.g., having a personal doctor, experiencing cost-related delays in seeking care or taking medications); care utilization (e.g., ED and office visits); preventive care (e.g., blood glucose or cholesterol check); quality of care (e.g., regular communications with a provider for a chronic condition); and overall health.
The Bottom Line
Both traditional Medicaid expansion and the private option, which uses federal funds to purchase private plans, improve the likelihood that low-income adults will be able to get insurance coverage, afford needed health care, and obtain regular care for chronic conditions.
