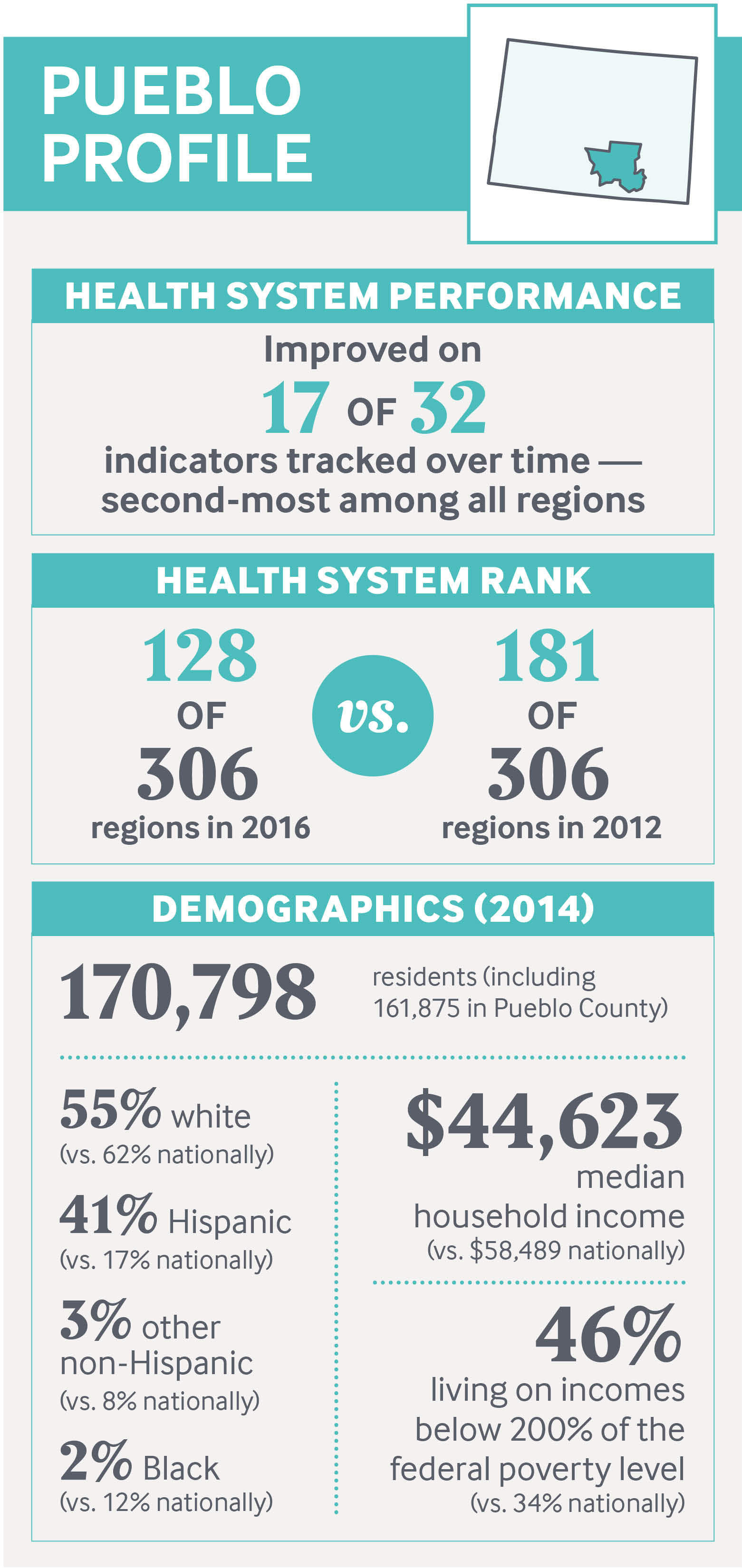
The high-desert region encompassing Pueblo in southeastern Colorado was one of only 14 out of 306 regions nationally to improve on a majority of performance measures tracked by the Commonwealth Fund’s Scorecard on Local Health System Performance, 2016 Edition. Socioeconomic challenges and geographic isolation have fostered a sense of interdependence among local health care providers, who have leveraged the state’s Medicaid expansion to enhance access to care while improving coordination. Providers have also joined with public health and social service agencies, businesses, educators, and nonprofits in creating the Pueblo Triple Aim Corporation, an improvement collaborative that uses data to define problems and create shared accountability for solving them. The group engaged the community in youth development programs as part of an effort that reduced the teen pregnancy rate by more than half. This and other collaborative efforts tap state policy to accomplish local priorities while seeking to build community pride.
Background
Data: D. C. Radley, D. McCarthy, and S. L. Hayes, Rising to the Challenge: The Commonwealth Fund Scorecard on Local Health System Performance, 2016 Edition, The Commonwealth Fund, July 2016; and American Community Survey, 2014 1-year estimates, www.factfinder.census.gov. Unless otherwise noted, data on the Pueblo hospital referral region are derived from the Scorecard.
The high-desert city of Pueblo, home to over 108,000 residents in southeastern Colorado, is a world apart from the buzzing economy that lines the Denver-to-Boulder corridor just a few hours north. Once known as the “Pittsburgh of the West,” the region evolved around the steel industry, with the largest mill owned by John D. Rockefeller. It suffered through many boom-and-bust cycles in the 19th and 20th centuries, but the collapse of the steel market in 1982 and the recent recession were the worst blows, shuttering all but one of the mills and draining away thousands of jobs. For the past several decades, many of the region’s residents have lived in generational poverty; nearly half (46%) subsist on incomes that are less than twice the federal poverty level.
Hispanics make up a large portion of the population (41%). One of four adults smoke and nearly a third are obese, both risk factors for diabetes, which is twice as prevalent among adults in Pueblo County as in Colorado (13.6% vs. 6.8%).1 Many residents suffer from disabilities, whether from the complications of disease, injuries from steel jobs, or self-harm due to substance abuse.2 Community leaders say that while Colorado’s legalization of marijuana has added jobs, it has also strained social services by attracting homeless and drug-seeking populations to the region, where the cost of living is lower than in other parts of the state.
This case study is part of a series exploring the factors that may contribute to improved regional health system performance. It describes how Pueblo’s health care provider organizations have joined forces with government agencies including the public health and fire departments, as well as business leaders, social service agencies, philanthropists, and educators to address the community’s health and social problems. Deliberate efforts to use data to define the problems and secure engagement from diverse leaders seem to have helped cut the teen pregnancy rate by half and curbed unnecessary hospital use, for example.
“There is a nucleus of people here who are exceptionally devoted to collaboration,” says Rev. Linda Stetter, director of mission and spiritual care for St. Mary–Corwin Medical Center, one of two hospitals in Pueblo. “I don’t think I’ve lived in another community where the collaboration is this intentional.” Such collaborative efforts build on providers’ commitment to health care quality improvement, first pursued in the 1980s at Parkview Medical Center, and subsequently taken up by other local institutions.3
It’s also notable that Pueblo’s economy has improved somewhat in recent years; its steelmaking equipment has been repurposed to recycle scrap metal and build wind turbines, and a large solar farm opened there in 2014. This recovery may have played a role in the improvements tracked in the Scorecard.

Health System Performance in Pueblo
The Pueblo hospital referral region (HRR), a regional market for health care, includes the city and surrounding Pueblo County as well as parts of adjacent counties.4 On the Commonwealth Fund’s Scorecard on Local Health System Performance, 2016 Edition, the region stands out for achieving significant improvements on a majority (17 of 32) of measures for which trend data exist. It was one of only 14 regions among 306 studied by the Scorecard to achieve this distinction — a finding even more notable given the region’s high poverty rate, since higher income usually correlates with better health and health care. The Scorecard found wide variation among HRRs on indicators of health care access, quality, avoidable hospital use, costs, and outcomes.
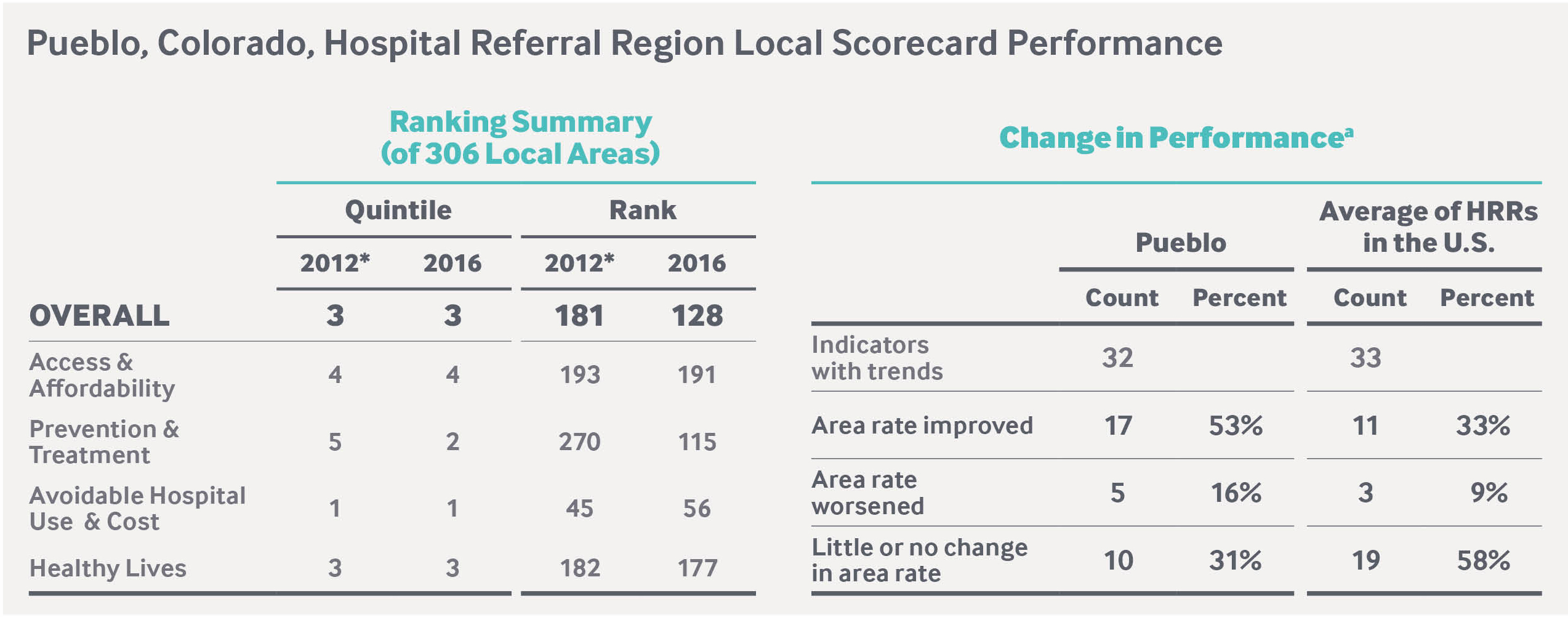
a Improved or worsened denotes a change of at least one-half (0.5) of a standard deviation (a statistical measure of variation) larger than the indicator’s distribution among all HRRs over the two time points. Little or no change denotes no change in rate or a change of less than one-half of a standard deviation. For complete results, visit the Health System Data Center.
Data: D. C. Radley, D. McCarthy, and S. L. Hayes, Rising to the Challenge: The Commonwealth Fund Scorecard on Local Health System Performance, 2016 Edition, The Commonwealth Fund, July 2016.
Delivery System: Spirit of “Co-Opetition”
Because of Pueblo’s relatively small size and geographic isolation, health care services tend to be concentrated within a few institutions, including two nonprofit hospitals: the independent Parkview Medical Center and St. Mary–Corwin Medical Center, part of the Centura network of faith-based hospitals. Together with Pueblo Community Health Center, a federally qualified health center (FQHC), and Health Solutions, a community mental health center, they are Pueblo’s safety net. At Parkview, for example, about 80 percent of admitted patients are covered by Medicare or Medicaid or are uninsured.

High demand for services, coupled with lean reimbursement and workforce shortages, foster interdependence among Pueblo’s health care organizations. A spirit of “co-opetition” — a willingness to work together to pursue common interests, while competing for patient loyalty — is evident in the two hospitals’ practice of sharing medical specialists, who are scarce resources in this region. Both have made a commitment not to divert patients from their emergency departments, since there is nowhere else for patients to go. Such efforts are enabled by routine meetings of the CEOs and an open-door policy among leaders at both institutions to discuss community concerns. “Both hospitals have a significant role to play to address the large community health burden in Pueblo,” says Matt Guy, former executive director of the Pueblo Triple Aim Corporation, a health care improvement collaborative, and now president of the consulting firm Accelerated Transformation Associates.
Expanding Access to Care

Local providers have worked to enroll people in health coverage, building on Colorado’s efforts to expand Medicaid. These began in 2010 with the institution of a hospital provider fee that draws additional federal matching funds to expand coverage to more low-income children and adults and enhance reimbursement to providers, thereby reducing uncompensated care.5 This has helped Pueblo’s safety-net hospitals expand access to care, while also rewarding them for improving quality. In 2014, Colorado further expanded Medicaid to more low-income adults through the Affordable Care Act.
While the Scorecard did not detect a substantial drop in the region’s uninsured working-age adult population from 2012 to 2014, the rate fell to 10 percent in 2015 — better than state (12%) and national (13%) rates.6 The Scorecard found improvements from 2011–12 to 2013–14 on two related indicators: an increase in the share of adults with a usual source of care (from 77% to 81%), as well as a steep decline in the share of at-risk adults who went without a physician visit in the past two years (from 21% to 13%) — in both cases besting state and national rates. Parkview may have contributed to this improvement by providing Pueblo County’s urgent care and emergency facilities with lists of local primary care physicians, information on school-based clinics, and health department resources to share with patients.
Health care providers have also expanded primary care capacity. In 2012, Parkview established an internal medicine residency program, which retained over half its graduates in its first two years. (This program complements a longstanding family medicine residency at St. Mary–Corwin.) The hospital also opened another primary care clinic and “leased” one of its staff endocrinologists to the FQHC for a few days each month, enabling easier access to this in-demand service. During the period the Scorecard measured, many of the practices affiliated with St. Mary–Corwin established themselves as patient-centered medical homes, part of an initiative to make after-hours care more available and chronic disease management and preventive services more accessible.7
Medicaid expansion also helped the FQHC hire more nurse practitioners and physician assistants to work on care teams in an expanded facility, thereby eliminating a waiting list for accepting new patients. Today the community health center is able to provide same- or next-day appointments for urgent issues and schedule most routine visits in less than 21 days, though it still faces capacity challenges given its difficulty in hiring primary care providers.8 Since 2009, it has operated five school-based clinics in a partnership with Parkview Medical Center that provide primary care, vaccinations, birth control, sports fitness exams, prescriptions, and referrals for specialty care.
Improving the Quality of Care
Pueblo’s most notable gains were on measures assessing the delivery of preventive care and evidence-based treatment. Improvements on 10 of 12 indicators vaulted the region from the fifth to the second quintile of performance on this domain. This progress suggests that quality improvement has become embedded in the local health care culture. This may be attributable, in part, to deliberate steps taken by Parkview Medical Center, which retains the largest market share in the region, to reduce variation and promote evidence-based care.9 Leaders say Parkview’s commitment to quality improvement — and national recognitions it received as a result — spurred others to improve. “Several thousand people visited to see what the hospital was doing,” says Michael Pugh, who served as CEO in the 1990s.
During the years tracked by the Scorecard, Parkview set goals to reduce patient harm and improve clinical quality and service, reporting progress monthly to all staff and its board.10 Among other efforts, staff members began checking on patients every hour and making bedside shift changes to promote clear and continuous communication among providers and between patients and providers.
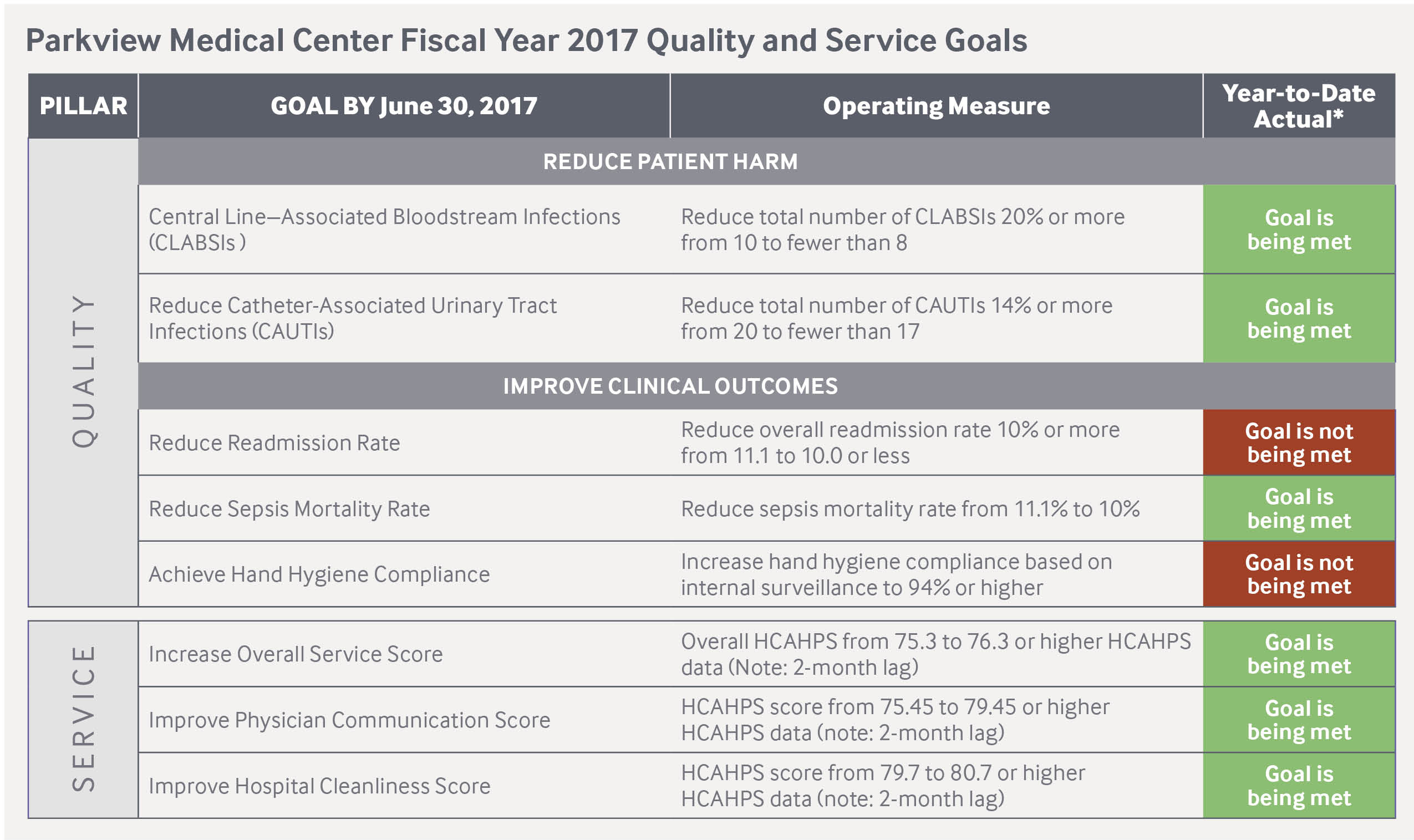
* Actual as of Sept. 2016.
Data: Parkview Medical Center.
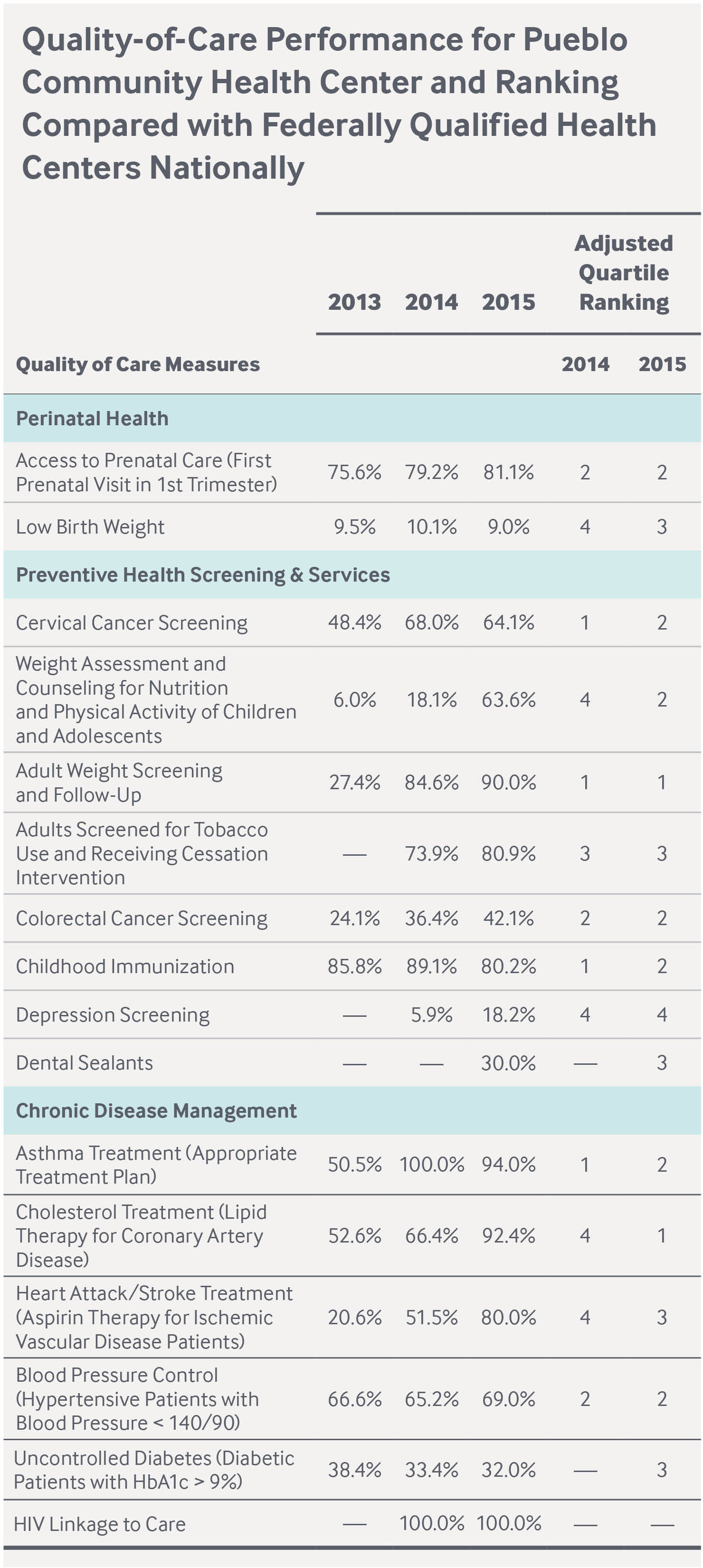
Data: HRSA Health Center Program, Pueblo Community Health Center 2015 Profile.
With incentives from public and private insurers to improve the quality of care, Pueblo Community Health Center has achieved its goal of performing above the national median among FQHCs for nine of 15 indicators tracked by the federal government. Through Colorado Medicaid’s Accountable Care Collaborative, created in 2010 to improve care while expanding coverage, the FQHC receives per member per month funding (in addition to fee-for-service reimbursement) to coordinate care for its 20,000 Medicaid patients. It uses a web-based system and claims data to identify gaps in care — for example missed postpartum appointments or well-child checks — and to work with frequent emergency department or hospital users to offer chronic care management and other support.11 In 2011, the FQHC received recognition as a medical home by the Accreditation Association of Ambulatory Health Care for its efforts to expand access and improve the quality of care.
Collaborative efforts to promote preventive care and to improve care coordination across settings have also been launched. Pueblo’s public health department partners with the residency programs at Parkview and St. Mary–Corwin to promote colorectal cancer screenings through a chart review and tracking system, which led to an increase in the number of adults screened.12 Case managers at the FQHC coordinate care for high-risk obstetric patients by scheduling appointments for them at St. Mary–Corwin’s high-risk obstetrics clinic, making sure they attend, and helping them adhere to recommended treatment.
COLLABORATING REGIONALLY TO COORDINATE CARE FOR MEDICAID PATIENTSColorado in 2010 created a Medicaid Accountable Care Collaborative (ACC) to promote care coordination and efficiency while expanding coverage for Medicaid beneficiaries.a The ACC comprises seven regional care collaborative organizations (RCCOs) selected by the state, which pays them a fee of up to $12 per member per month (PMPM) to oversee medical management, provider network development and support, and performance reporting. RCCOs contract with primary care providers, who receive $3 PMPM from the state (on top of fee-for-service reimbursement) for participating in care coordination and quality improvement activities. Both may also earn financial incentives for meeting performance targets. 
Donald Moore, CEO of Pueblo Community Health Center, says Colorado’s Medicaid Accountable Care Collaborative has enabled the health center to invest in the infrastructure needed to coordinate patient care.
Integrated Community Health Partnership, LLC, is the RCCO serving Pueblo and 18 other counties in southeastern Colorado. Its members include a behavioral health organization and four community mental health centers as well as a consortium of three FQHCs.b The RCCO passes a portion of its fee to the FQHCs to coordinate care for their Medicaid patients and to the community mental health centers (Health Solutions in Pueblo) to coordinate care for other Medicaid beneficiaries. For example, Health Solutions hired 10 registered nurses to serve as patient advocates and navigators primarily on behalf of dually eligible Medicare and Medicaid clients. They spend time in providers’ practices and connect clients to resources to meet their medical and nonmedical needs. To date, the most beneficial aspect of the RCCO has been to bring the partners together to identify what is and isn’t working in their communities, according to Chris Senz, CEO of Integrated Community Health Partnership. The program has enabled FQHCs such as the Pueblo Community Health Center to create a care coordination infrastructure that was not possible under traditional fee-for-service reimbursement, according to Donald Moore, its CEO. The ACC program saved an estimated $37 million statewide in fiscal 2014–15, according to the state of Colorado.c a D. Rodin and S. Silow-Carroll, Medicaid Payment and Delivery Reform in Colorado: ACOs at the Regional Level (The Commonwealth Fund, March 2013). |
Since 2001, the FQHC has been the first point of contact for hospitals when they discharge patients who do not have an identified source of primary care. In recent years, Parkview added a dedicated team to contact patients after discharge to ensure they understand their treatment plan and have a follow-up appointment scheduled. In 2015, the Southeastern Colorado Transitions of Care Consortium (launched by the Pueblo Triple Aim Corporation) brought together Pueblo’s urban and regional hospitals, community mental health center, and the FQHC, physician groups, insurers, and the Medicaid Regional Care Collaborative Organization to align and improve their care coordination efforts.
Pueblo’s fire department has joined the consortium, prompted by a growing number of 911 calls, which increased from 2,000 in 2008 to 21,000 in 2015. Some came from residents who would repeatedly fall in their homes; others came from people who simply needed a way to access the health system.13 This resulted in the 2016 launch a pilot program called Directing Others to Service, or DOTS, in which fire department staff and providers connect frequent users of the emergency response system with medical homes or other sources of help. Fire department staff also visit frequent 911 callers to identify needs — such as a grab bar in their bathroom or an eyeglass prescription — that could be addressed to head off future emergencies.14
Addressing Social Determinants
Pueblo’s health care providers have also moved to address the social determinants of poor health, including poor nutrition. In response to evidence that 17 percent of Pueblo residents lacked access to healthy food, St. Mary–Corwin in 2013 launched a farm stand in its own neighborhood, which is considered both a food desert because of its lack of healthy food options and a food swamp because of its abundance of cheap, low-nutrition options.15 The hospitals’ physicians are able to write prescriptions for high-risk patients, including those who are obese and/or diabetic, to receive free fruit and vegetables there.16 Parkview has also sought to promote better nutrition by sending nurses to worksites and public venues to offer dietary advice and free diabetes screenings. Such work is reinforced by the public health department’s efforts to help local food retailers purchase freezers or make other changes necessary to sell healthier products, and successful lobbying of Walmart to open a store in one of Pueblo’s poorest neighborhoods.
ENGAGING FAITH COMMUNITIES, TRYING COMPLEMENTARY APPROACHESWhen Rev. Linda Stetter came to Pueblo to become the director of mission and spiritual care for St. Mary–Corwin Medical Center in 2013, she started church-hopping on Sundays. Thus far she’s visited more than 90 of the city’s 125 churches. Having worked in communities with strong interfaith associations, Stetter knew that religious leaders could serve as community partners for hospitals such as hers — offering pastoral care to sick members of their congregations or speaking to congregants about good nutrition and other healthy behaviors. She began offering quarterly symposia to clergy on such topics and now receives requests from them to be educated about issues like autism that are of concern to their congregants. 
Rev. Linda Stetter, director of mission and spiritual care for St. Mary–Corwin Medical Center, at the hospital’s farm stand. St. Mary–Corwin physicians can write prescriptions for patients to receive free fruit and vegetables.
Stetter hopes to try the Memphis Model in Pueblo, an approach developed at Methodist Le Bonheur Healthcare in Memphis, Tenn. Through the hospital’s Congregational Health Network, members of some 500 Memphis churches, many African American, have agreed to help chronically ill congregants, in part by checking up on them after hospitalizations. “They are cared for like neighbors used to care for neighbors,” says Stetter. Methodist Le Bonheur has reported that over a three-year period patients served through this network had shorter hospital stays, longer intervals between hospitalizations, and significantly lower mortality rates.a Stetter also helps direct St. Mary–Corwin’s use of complementary therapies such as acupuncture and mindfulness in the intensive care unit, emergency department, and elsewhere to help those dealing with addiction, pain, and stress. Such approaches have been especially needed to help the hospital’s pain management clinic treat a population of opioid-dependent patients. In 2007 two local doctors were forced to close their practices over alleged overprescribing, and Pueblo has received negative publicity as the highest drug-prescribing city in Colorado.b The hospital’s commitment to complementary therapies — including the services of a harpist — is an effort “to help people cope with their chronic illnesses and their mental conditions beyond the hospital walls,” says Stetter. a A. Halperin, “It Really Does Take a Village: How Memphis Is Fixing Healthcare,” Salon, Sept. 3, 2013. |
St. Mary–Corwin has also partnered with the city to enforce code violations against landlords for problems that impact health, like mold and bug infestations. And Stetter has led an effort to educate Pueblo’s religious leaders about health issues and enlist them in supporting members of their congregations.
Collective Action Across Sectors
Several leaders note that Pueblo has a history of collaborative efforts, most notably the One Community Pueblo initiative, begun in 2008, involving health providers, educators, law enforcement officials, and judges in supporting healthy child and youth development, in part by promoting access to mental and physical health services. The effort involves collecting extensive data and reporting it on a public dashboard.17
In 2010, Pueblo’s two hospitals conducted their first community health needs assessments, a requirement for nonprofit institutions under the Affordable Care Act, and the public health department created a new community health improvement plan. These analyses cast into stark relief the breadth and depth of Pueblo’s health problems and prompted leaders to move beyond ad hoc efforts to take collective action. After hearing about the Institute for Healthcare Improvement’s Triple Aim — for improved care, improved population health, and reduced per capita costs — leaders founded the Pueblo Triple Aim Corporation, a nonprofit with a dedicated staff and infrastructure.18 Leaders from the business community, social services, philanthropy, economic development, and education, as well as Latino and other community groups, have joined.
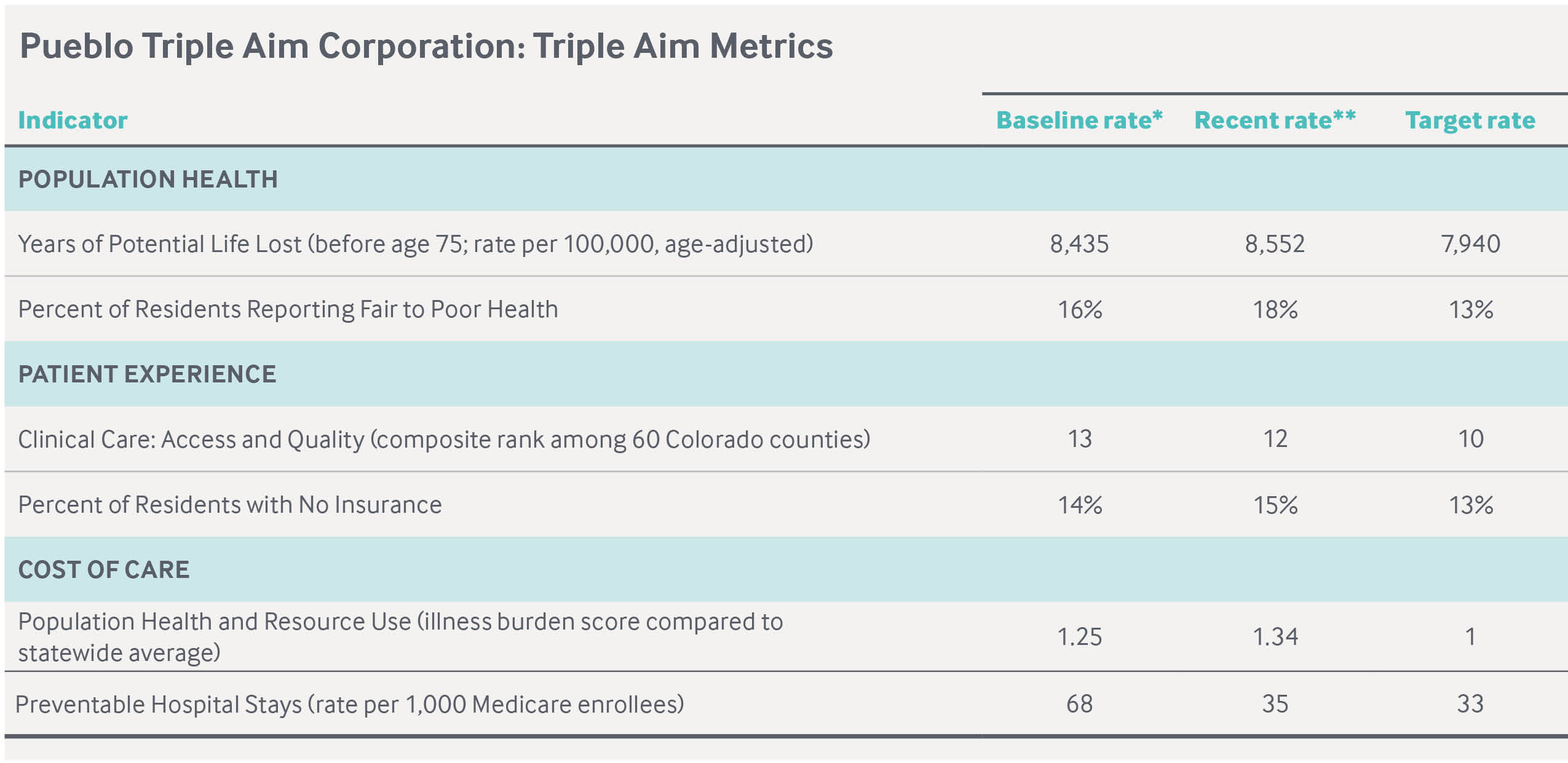
** Recent rate represents the 2016 reporting year, except for Population Health and Resource Use (illness burden score compared to statewide average), which represents the 2012 reporting year.
Data: Triple Aim Measures (Pueblo Triple Aim Corporation, n.d.).
The group uses a data dashboard to track key population health indicators for Pueblo County residents, compare Pueblo’s performance with other counties, and set goals for improvement.19 At this stage, some targets — such as a reduction in the premature death rate — appear to be largely aspirational, while others — such as reducing the rate of preventable hospitalizations — may be influenced in part by initiatives such as the care transitions consortium described above.
To guide their work, members worked with the ReThink Health initiative, a nonprofit promoting regional health improvement, to model the long-term effects of various health policies on Pueblo residents’ lives, health care costs, quality of care, equity, and productivity.20 This exercise helped convince employers facing rising health costs and overburdened safety-net providers that making long-term and even modest investments in better health could yield significant financial returns. “The big thing that became evident through the modeling was that to have impact they would have to move upstream and look at those social determinants of health,” says Randy Evetts, senior program officer for the David and Lucile Packard Foundation, which financed the development of the dashboard and supports a number of causes in Pueblo, the birthplace of David Packard, Hewlett-Packard’s cofounder. The Pueblo Triple Aim Corporation has leveraged grants from a number of foundations to fund its work.21
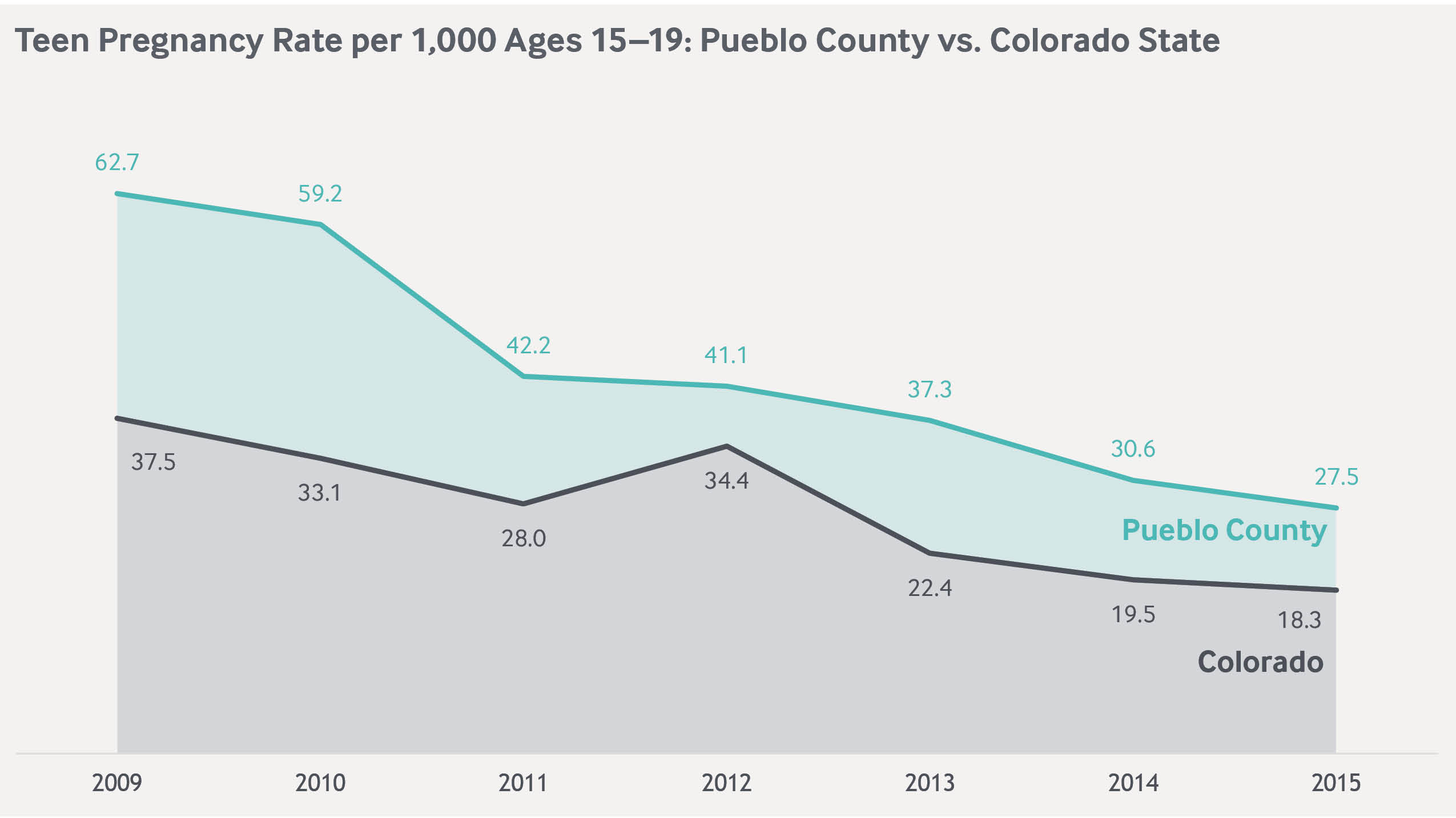
The group’s initial effort, led by the public health department, sought to reduce teen pregnancy rates, which for years were among the highest in the state. Past efforts to address the issue had splintered, in part over disagreements about whether to promote contraception or abstinence-only approaches (many in the community identify as Catholic or evangelical Christian).22 Cognizant of this history, the Triple Aim group recast the issue as not just preventing pregnancies but promoting positive youth development — including mentoring initiatives, efforts to educate teens about their career options, and a sexual health educational campaign.23

The community’s effort to reduce teen pregnancy gained momentum from Colorado’s groundbreaking policy to make long-acting reversible contraception (LARC) free to low-income teenagers and women through family planning centers, which led to a 50 percent drop in the state’s teen pregnancy rate from 2009 to 2015.24 Pueblo County more than halved its rate during this time, representing a much larger decline in absolute terms (a reduction of 35.2 per 1,000 in Pueblo vs. 19.2 per 1,000 for the state). The local public health department helped promote use of LARC, in part by talking to providers. “We found that teens were very scared and reluctant to even come in to a clinic and talk about their sexual health,” says Sylvia Proud, director of Pueblo City-County Health Department. “We have done a lot with how to talk to teens, how to make clinics more teen-friendly environments.”
Members of the Pueblo Triple Aim Corporation are also working to increase healthy behaviors and reduce obesity. Pueblo was the first Colorado city to ban smoking in public spaces; the group is now working with the housing authority to make low-income housing units smoke free. The organization also participates in national learning collaboratives on health improvement.25

Lessons
Cross-sector coalitions can help communities build the will needed to take collective action. The Pueblo region has worked to create a positive identity in the face of long-standing social problems that can wear down the spirit of volunteerism over time. Improvement efforts have gained traction in recent years as community leaders have found common ground, helped to a great extent by coalitions such as the Pueblo Triple Aim Corporation.26 Cross-sector efforts have built on one another to develop leaders’ capacity for public–private collaboration, nurtured by financial support from foundations, local charities, and an insurer. To make progress in a collaborative way, community leaders need to cultivate a sense of “patient urgency,” says Guy, by slowly building trusting relationships while immediately taking incremental steps toward achieving agreed-upon goals for improvement.
Supportive state policies lay the groundwork for local improvement. Pueblo has benefitted from supportive state policy, most notably Colorado’s health care reforms that expanded Medicaid before and after enactment of the Affordable Care Act, as well as the creation of the Medicaid Accountable Care Collaborative and policies such as support for the use of long-acting reversible contraceptives. But the grassroots efforts led by Pueblo’s community leaders have ensured there is fertile ground for localizing state policy to serve the priorities of this independent region, which can be wary of receiving dictates from state government. “There is a very fierce Pueblo culture of, ‘We are going to do it our way,’” says Guy. “We will take your help, but this is our community, and we are going to do it our way.”

